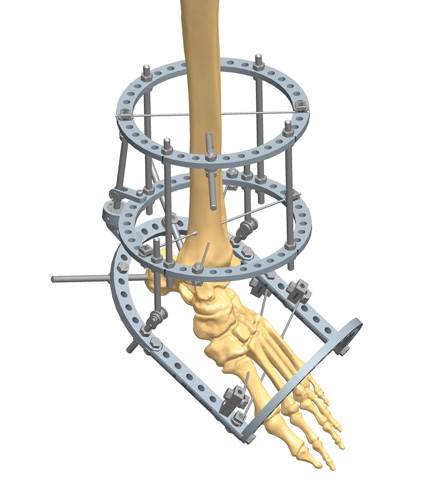
TrueLok™ Fixator
THIS INFORMATION IS FOR HEALTHCARE PROFESSIONALS ONLY
THIS INFORMATION IS FOR HEALTHCARE PROFESSIONALS ONLY
Equinus deformity treated with TrueLok Fixator.
| Q.ty | Catalogue N. | Description |
|---|---|---|
| 2 | 56-10920
|
TL PLUS FULL RING, 150MM |
| 1 | 56-13620
|
TL PLUS FOOTPLATE 150MM |
| 2 | 56-14590
|
TL+ FOOT PLATE EXTENSION 5 HOLE |
| 1 | 56-11620
|
TL PLUS HALF RING 150MM |
| 4 | 55-10070
|
165MM THREADED ROD |
| 10 | 54-1152
|
TL,BOLT, WIRE FIXATION, UNIVERSAL |
| 3 | 54-11530
|
TL+ UNIVERSAL HALF PIN FIXATION BOLT 4MM - 6MM |
| 1 | 51-10470
|
TL+ ANGULAR DISTRACTOR 150MM |
| 2 | 51-10430
|
TL+ CANNULATED INLINE HINGE ASSEMBLY |
| 2 | 55-10530
|
85MM THREADED ROD |
| 2 | 54-11600
|
TL+ ONE HOLE POST |
| 1 | 54-11610
|
TL+ TWO HOLE POST |
| 6 | 54-1010
|
TL,BOLT, 16MM |
| 41 | 50-1008
|
TL, NUT, STAINLESS STEEL, 10MM |
| 3 | 54-1216
|
TL,WIRE, BAYONET, 1.8MM X 400MM |
| 2 | 54-1215
|
TL,WIRE, W/STOPPER, 1.8MM X 400MM |


Foot and Ankle Charcot Reconstruction with External Fixation
Surgical reconstruction of foot and ankle Charcot with external fixation is especially useful in the presence of poor bone quality,Read MoreExpert Tips on How to Medically Diagnose Charcot Arthropathy
The diagnosis of Charcot neuroarthropathy of the foot and ankle can be challenging due to a lack of information inRead MoreThis website is reserved only for Healthcare Professionals and their staff. Therefore, the access to these information is denied to non professional audience.