Charcot neuroarthropathy is a rare, but devastating complication of diabetes1. Progressive destruction of the bones and joints of the foot cause deformities and thus alter foot biomechanics1. If not recognized nor treated properly, the disease can result in ulcer formation, infection, and progression of the disease with joint instability and bone destruction2,3. In the worst case, limb amputation is required4,5.
In this article, we will focus on the foot biomechanics, challenges of Charcot foot surgery and briefly describe different surgical approaches.
Foot Biomechanics
The most common foot bone anatomies involved in the Charcot neuroarthropathy are6:
- The Lisfranc joint: articulation between the midfoot and forefoot; affected in about 60% of cases.
- The Chopart joint: transverse/midtarsal joint (talus and calcaneus proximally, navicular and cuboid bone distally); affected in about 30% of cases.
- The ankle joint: affected in about 10% of cases.
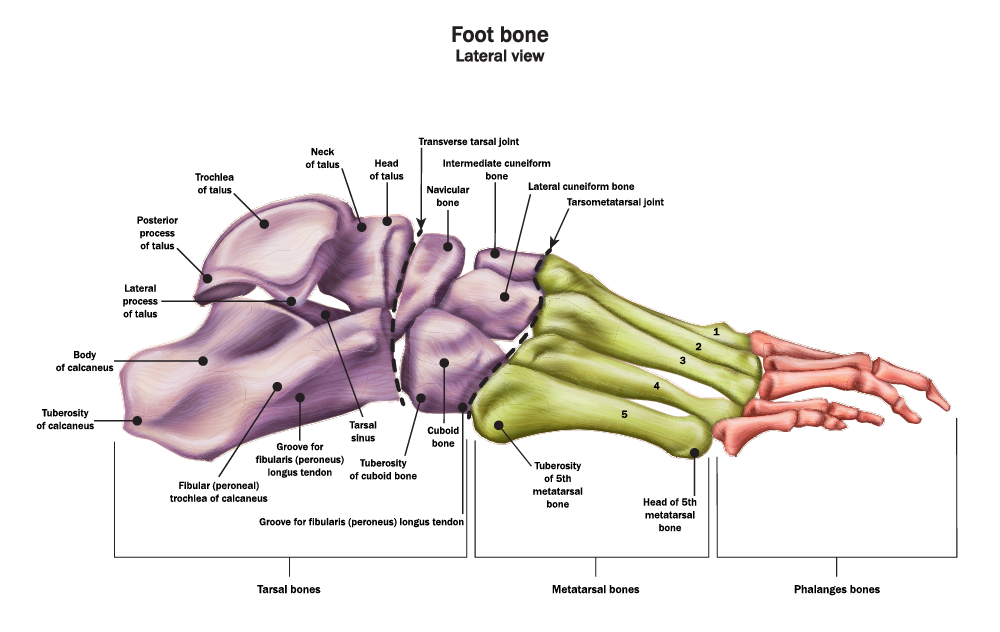
In patients with advanced stages of the disease, the involved joints collapse, and the foot takes on an abnormal shape, such as the rocker bottom appearance shown in Figure 1.
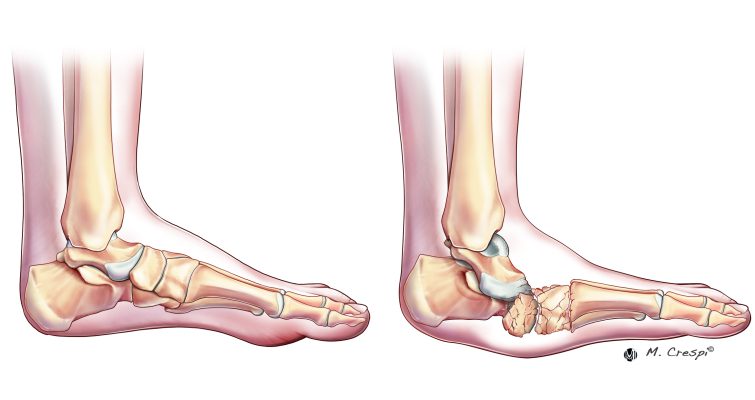
Figure 1 – Differences in appearance between normal foot and Charcot foot6
The altered joint morphology – a result of osteopenia and lack of proprioceptive feedback – increases mechanical forces, leading to further joint deterioration in a negative feedback loop.
Indications for Charcot Foot Fixation
The main goal of Charcot foot treatment, independent of the approach, is to achieve a stable plantigrade foot resistant to ulceration, prevent amputation, and improve the patient’s quality of life7. Untreated deformities may cause ulcers with the risk for deep infection and subsequent amputation. Lower limb amputation, in turn, significantly impacts patients’ lives8. Partial foot amputation was reported to result in mortality rates of 22% after 1 year, whereas transtibial or more proximal amputations can reach mortality rates as high as 52% after 1 year8.
Therefore, surgical reconstruction should be considered in the presence of the following6:
- Severe instability of the foot or ankle
- Varus or valgus deformity of the foot or ankle
- Acute dislocation of the foot or ankle
- Infected, long standing and recalcitrant ulcers
- Failure of previous conservative treatment.
Patients with an unstable ankle in the coronal and sagittal plane are very prone to ulceration and require rapid surgical reconstruction. Daniel Scott (MD, Medical University of South Carolina (MUSC) Orthopaedics, Charleston) confirms: “Every time I see a patient with Charcot of the ankle, I’m a lot more worried. These patients are prone to ulceration and require rapid surgery when the coronal and sagittal plane show an unstable ankle.”
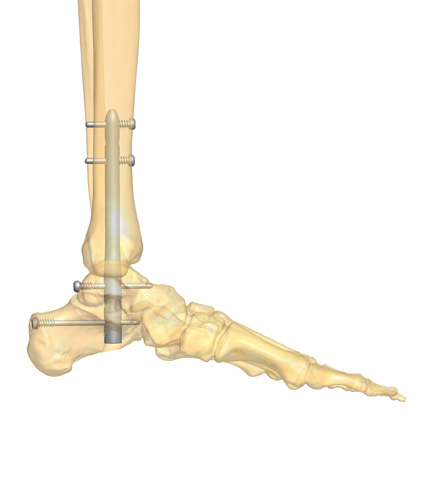
The most common methods of Charcot foot fixation are internal fixation, external fixation, or a combination of both9. The success of Charcot foot surgery, however, can be compromised by various factors, including:
- Delayed wound healing and infection
- impacted by immune dysfunction, hyperglycemia, and nutritional and biologic deficiencies
- Delayed bone healing due to neurovascular and autonomic dysfunctions
- along with inflammation and trophic alterations to bone9.
Therefore, the combination of altered bone healing, decreased bone density, poor soft tissue envelope, and recurrent progressive fracture patterns create significant challenges for surgical fixation methods9.
Internal Fixation
Charcot-specific fixation systems have evolved to address the mechanical demands on internal fixation constructs due to bone resorption, fragmentation, and osteoporosis9,10. Internal fixation methods include plating with locking screws, axial beaming with solid bolts and screws, and retrograde hindfoot intramedullary nailing10.
As standard plating is usually insufficient for Charcot foot reconstruction, the principle of superconstructs was first described by Sammarco et al. (2009). It is defined by 4 factors7:
- Fusion is extended to non-affected joints for better fixation.
- Bone resection to shorten the extremity is performed to allow adequate reduction without undue tension on the soft tissue envelope.
- The strongest implant, as tolerated by the soft tissue envelope, is selected.
- In particular, biomechanical studies of Charcot-specific implants showed higher stiffness, force to failure, and pullout strength for stainless steel than for titanium11.
- Implants are positioned in a way to maximize mechanical function.
Midfoot beaming allows for restoring the medial and lateral columns with minimal soft tissue dissection10. Beaming can be performed with screws or bolts and resists axial loading forces across the midtarsal joints10. However, the risk of hardware failure after beaming should be considered. Hardware failure rates reported in scientific literature vary from 4% to 67%12-14.
Mohammad Sharif (DPM, Village Podiatry, Atlanta) explains his beaming approach: “My surgical approach always includes beaming. Beaming of the medial and lateral column is usually considered for midfoot pathologies, whereas the subtalar joint is included when the rear foot is also involved.”
Intramedullary nail fixation is used for hindfoot and ankle reconstruction, with tibiotalocalcaneal (TTC) arthrodesis being the most common technique10. Retrograde intramedullary nailing offers a stable load-sharing fixation that resists torsional forces10.
External Fixation
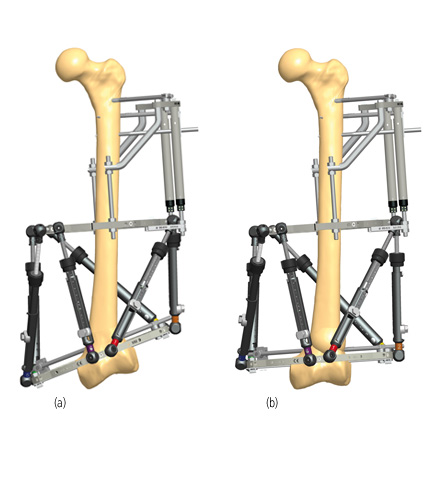
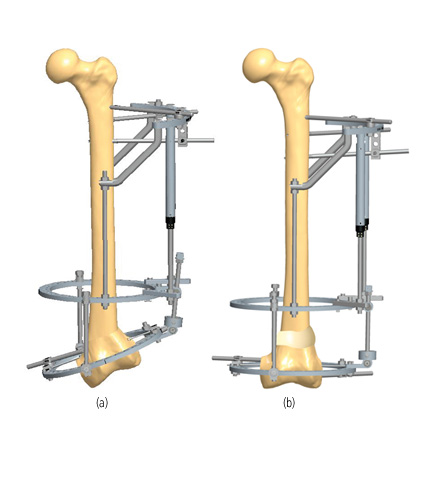
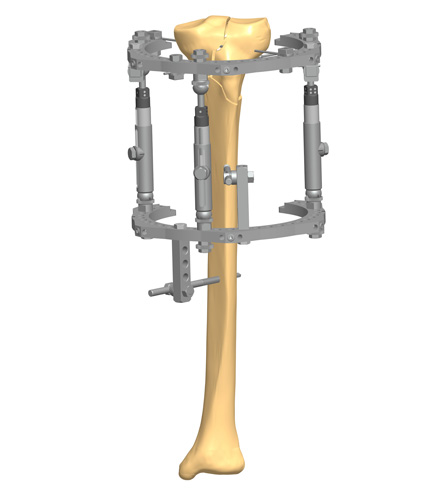
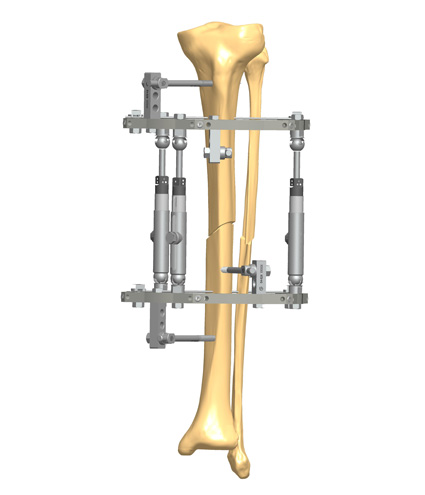
External fixation is especially useful in the presence of poor bone quality, ulceration, compromised soft tissue, active infection, or osteomyelitis, where the use of internal fixation is limited or contraindicated10. Circular external fixation is the most described external fixation method as it allows deformity correction while providing stability and compression when arthrodesis is required9. Compared to monolateral external fixators, circular external fixators do not rely on the cortical fixation of half pins but gain stability through transosseous wires9. They are suitable for midfoot, rearfoot, and ankle deformities9. An overview of different concepts of circular external fixation is shown in Table 1.
Table 1 Characteristics of circular external fixation concepts9
Circular External Fixation Concept |
Characteristics |
| Static circular external fixation | Provide primary stability or can augment fixation Can be prebuilt and are thus easy to use Example: combination of 2 tibia circular rings and a foot plate |
| Stabilization off-loading | Different designs, including hybrid constructs with circular rings and a bar-to-clamp apparatus Suitable to off-load wounds and for soft tissue reconstruction Off-loading constructs can be converted to a static or dynamic external fixation construct Example: tibia and forefoot ring connected with threaded rods |
| ADynamic external fixation | For severe long-standing deformities requiring staged correction Examples: Ilizarov technique or hexapod systems Allows continuous postoperative adjustment and thus prevents over- or undercorrection |
The most common complications associated with external fixation are pin site infections, pin/wire fixation failure, deep infection, malunion or nonunion9. Besides surgical experience, the outcome also highly depends on appropriate patient selection, continuous patient education, family support, and regular follow-up by a multidisciplinary team9.
Combined Internal and External Fixation
Severe obesity, a need for increased mechanical stability and/or soft tissue protection, control of adjacent joint mobility, and a high risk for hardware failure are the main indications for a combined internal and external fixation approach9. Internal fixation for midfoot correction combined with external fixation can be used to address an equinus contracture. In the presence of unstable rearfoot or ankle deformities, the combination of plate fixation or intramedullary nailing with external fixation can provide proper alignment while providing compression and limited motion for better bone healing9.
Best Practice Tips and Pitfalls
- Patients with diabetic neuropathy have difficulties in adhering to long periods of non-weightbearing. Therefore, robust and durable constructs are even more important than in non-diabetic and non-neuropathic patients15.
- In patients with midfoot pathologies, the placement of both a medial and lateral beam can prevent recurrent midfoot deformity16. Additional beams can be considered to improve postoperative outcomes16. You can find more information about beaming of midfoot pathologies here.
- In patients with combined midfoot and hindfoot pathologies, a combination of a hindfoot nail, midfoot beams and locking plates is used in modern approaches17. When using this combination, make sure that the hindfoot nail is inserted outside of the medial third of the talus as this area is reserved for medial column beam17.
Further Reading
Selecting the right surgical technique for Charcot foot fixation is challenging. Proper patient selection and addressing the patient’s comorbidities can significantly impact treatment success.
To help you prepare the best surgical approach for your Charcot cases we have compiled some Charcot foot surgical cases, which are available here.

References
1. Johnson-Lynn SE, McCaskie AW, Coll AP, Robinson AHN. Neuroarthropathy in diabetes: pathogenesis of Charcot arthropathy. Bone Joint Res. May 2018;7(5):373-378. doi:10.1302/2046-3758.75.Bjr-2017-0334.R1
2. Frykberg RG, Belczyk R. Epidemiology of the Charcot Foot. Clinics in Podiatric Medicine and Surgery. 2008/01/01/ 2008;25(1):17-28. doi:https://doi.org/10.1016/j.cpm.2007.10.001
3. Wukich DK, Sung W, Wipf SAM, Armstrong DG. The consequences of complacency: managing the effects of unrecognized Charcot feet. Diabetic Medicine. 2011;28(2):195-198. doi:https://doi.org/10.1111/j.1464-5491.2010.03141.x
4. Marmolejo VS, Arnold JF, Ponticello M, Anderson CA. Charcot Foot: Clinical Clues, Diagnostic Strategies, and Treatment Principles. Am Fam Physician. May 1 2018;97(9):594-599.
5. Trieb K. The Charcot foot. The Bone & Joint Journal. 2016;98-B(9):1155-1159. doi:10.1302/0301-620x.98b9.37038
6. Salvaterra P. The Surgical Management of Neuropathic (Charcot) Foot – A Practical Guideline. 2017;
7. Sammarco VJ. Superconstructs in the treatment of charcot foot deformity: plantar plating, locked plating, and axial screw fixation. Foot Ankle Clin. Sep 2009;14(3):393-407. doi:10.1016/j.fcl.2009.04.004
8. Fortington LV, Geertzen JH, van Netten JJ, Postema K, Rommers GM, Dijkstra PU. Short and long term mortality rates after a lower limb amputation. Eur J Vasc Endovasc Surg. Jul 2013;46(1):124-31. doi:10.1016/j.ejvs.2013.03.024
9. Stapleton JJ, Zgonis T. Surgical reconstruction of the diabetic Charcot foot: internal, external or combined fixation? Clin Podiatr Med Surg. Jul 2012;29(3):425-33. doi:10.1016/j.cpm.2012.04.003
10. Brandão RA, Weber JS, Larson D, et al. New Fixation Methods for the Treatment of the Diabetic Foot: Beaming, External Fixation, and Beyond. Clin Podiatr Med Surg. Jan 2018;35(1):63-76. doi:10.1016/j.cpm.2017.08.001
11. Wukich DK, Liu GT, Raspovic K, Vicenzi F. Biomechanical Performance of Charcot-Specific Implants. J Foot Ankle Surg. May-Jun 2021;60(3):440-447. doi:10.1053/j.jfas.2020.05.016
12. Ford SE, Cohen BE, Davis WH, Jones CP. Clinical Outcomes and Complications of Midfoot Charcot Reconstruction With Intramedullary Beaming. Foot Ankle Int. Jan 2019;40(1):18-23. doi:10.1177/1071100718799966
13. Grant WP, Garcia-Lavin S, Sabo R. Beaming the columns for Charcot diabetic foot reconstruction: a retrospective analysis. J Foot Ankle Surg. Mar-Apr 2011;50(2):182-9. doi:10.1053/j.jfas.2010.12.002
14. Butt DA, Hester T, Bilal A, Edmonds M, Kavarthapu V. The medial column Synthes Midfoot Fusion Bolt is associated with unacceptable rates of failure in corrective fusion for Charcot deformity: Results from a consecutive case series. Bone Joint J. Jun 2015;97-b(6):809-13. doi:10.1302/0301-620x.97b6.34844
15. Kummen I, Phyo N, Kavarthapu V. Charcot foot reconstruction—how do hardware failure and non-union affect the clinical outcomes? Annals of Joint. 2020;5
16. Grant W, Grant-McDonald L. Beaming the Charcot Foot. Clin Podiatr Med Surg. Oct 2022;39(4):605-627. doi:10.1016/j.cpm.2022.05.007
17. Kavarthapu V, Guduri V, Hester T. Combined Charcot hindfoot and midfoot reconstruction using internal fixation method—surgical technique and single surgeon series. Annals of Joint. 2023;8
Link to the Charcot article about internal fixation.
Link to Charcot article “Charcot Foot Reconstruction Using Internal Fixation”
Link to the downloadable premium material: “Neuropathic (Charcot) Foot surgical cases”.