Diabetic foot is one of the most important sources of morbidity in patients with diabetes, affecting 6.4% of patients worldwide. It is the most common cause of lower extremity amputation.
Complications from diabetic feet, including ulceration and Charcot Foot and Ankle, are a leading cause of hospitalization, resulting in high disease burden, poor quality of life, and increased healthcare costs. Notably, less than one-third of physicians recognize the signs of diabetes-related peripheral neuropathy and diabetic foot problems, even when the patient is symptomatic.
To improve diagnostic awareness, this article explores the most recent diabetic foot data. It will also focus on the symptoms and key elements to prevent foot ulcers and manage Charcot Foot and Ankle.
Diabetic Foot Data
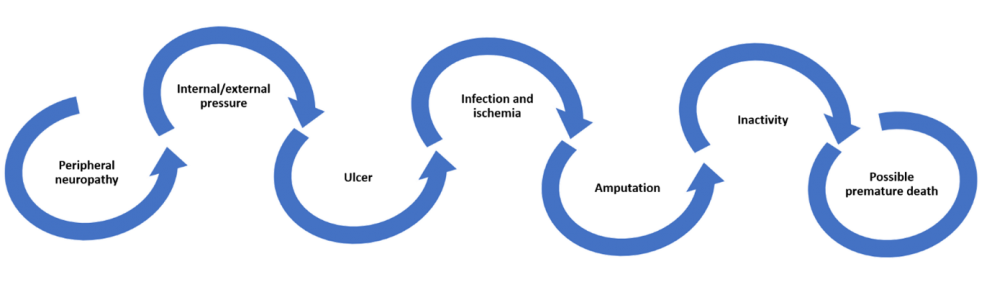
Diabetic foot and ankle problems are caused by peripheral neuropathy, particularly in the feet, which alters sensory function. Under these conditions, external trauma or internal bone pressure result in the development of ulcers.
According to the International Diabetes Federation, about 2% of people with diabetes suffer from foot ulceration annually. Chronic ulceration, when accompanied by ischemia and infection, dramatically increases the risk of major amputation. Lower limb amputation in people with diabetes is 10 to 20 times more common compared to those without diabetes. Still, with timely diagnosis and appropriate treatments, it is possible to prevent 4 out of 5 amputations.
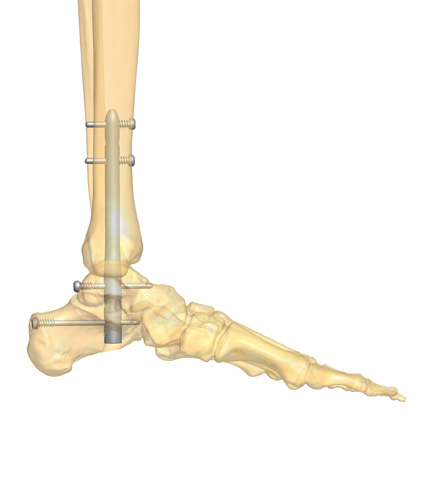
The nerve damage and poor circulation in diabetic feet can also lead to Charcot Foot and Ankle, especially in patients with poorly controlled blood sugar levels.
To further explore the diagnostic approach in the diabetic foot and its complications, read “The Stages of Charcot Foot and Ankle Disease and The Importance of a Quick Diagnosis.”
Diabetic Foot Symptoms
Diabetic foot complications are severe and chronic, with the potential to quickly evolve to a critical clinical state. Therefore, a timely diagnosis is essential. Here are some of the things to look for when screening at-risk feet:
- Warmth, swelling, redness or pain on foot and/or ankle
- Higher temperature of one foot compared to the other one (2°C or 4°F)
- Continuous unpleasant odor from the foot
- Skin lesions, ulcers and open/bleeding wounds
- Discolored, ingrown nails
- Infections
- Loss of foot sensitivity
- Corns, calluses, and dry cracks in the skin
Early recognition of Charcot Foot and Ankle may be difficult in early stages, but frequent monitoring of signs and symptoms and patient education play a crucial role in protecting feet at risk.
Key Elements for Preventing Foot Ulcers
Recent data has shown that up to 34% of type-2 diabetes patients may develop diabetic foot ulcer once in their lifetime, increasing their already high disease burden. But research also shows that foot ulceration is a complication of diabetes that can be prevented. The International Working Group on the Diabetic Foot Guidelines 2019 highlight five key elements that underpin prevention of diabetic foot problems:
- Identifying the at-risk foot, by performing an annual examination that includes vascular examination and assessment for sensory neuropathy.
- Regularly inspecting and examining the at-risk foot, paying special attention in patients with loss of protective sensation or peripheral artery disease.
- Educating patients, family and healthcare professionals about foot care. The aim is to improve a patient’s self-protective behavior and to facilitate adherence.
- Ensuring routine wearing of appropriate footwear, and referring the patient for special footwear, if necessary.
- Treating risk factors for ulceration, such as removing calluses, appropriately treating ingrown or thickened nails, and prescribing antifungal treatment for fungal infections.
Ulcer prevention remains a neglected opportunity, and lifelong surveillance is essential to protect feet at risk from ulceration.
Conclusion
Understanding the diabetic foot and taking the appropriate measures to detect and treat complications as soon as they arise go a long way in the prevention of limb amputation in patients with diabetes. Apparently minor injuries can quickly escalate into a critical situation, leading to emergency situations that require a drastic clinical approach.
To further explore the diagnostic approach in the diabetic foot and its complications, read “The Stages of Charcot Foot and Ankle Disease and The Importance of a Quick Diagnosis.”

References
- IDF Diabetes Atlas, 9th edition 2019
- Uccioli L et al Emergency Med 2013, 3:6.
- Caputo GM et al. Am Fam Physician. 1998 Jun 1;57(11):2705-2710.
- Pendsey SP Int J Diabetes Dev Ctries. 2010 Apr-Jun; 30(2): 75–79.
- Miranda C and Ros RD Transl Med UniSa. 2020 May; 22: 50–51.
- IWGDF Guidelines on the prevention and management of diabetic foot disease. 2019.