MORE POSTS
Surgical Management of the Charcot Ankle2024-01-17
Charcot neuroarthropathy of the ankle is an especially challenging condition that often leads to instability and destruction of the joint with significant morbidity requiring an amputation in many instances1-3. According to Brodsky et al., the ankle is affected in 9% of patients with Charcot neuroarthropathy, whereas the hindfoot is involved in 30-35%3. The overall goal of Charcot ankle reconstruction is to achieve a painless, plantigrade and stable foot, and thus avoid ulceration with subsequent infection1,2. However, this procedure is also associated with a high complication rate1,2.
Postoperative Management in Charcot Foot Reconstruction2024-01-10
The successful treatment of Charcot foot does not end with a completed surgery; success also requires a diligent postoperative care regime. This devastating condition mainly affects patients with diabetes and peripheral neuropathy, resulting in bone destruction and joint deformation1. During the initial, inflammatory stage, the recommended treatment consists of off-loading with total contact casts or custom orthotics to prevent further damage, although surgical management is indicated in cases of severe instability or soft tissue compromise2. After the acute stage, the focus of treatment is on deformity correction and foot reconstruction to prevent further damage and improve the patients’ quality of life2.
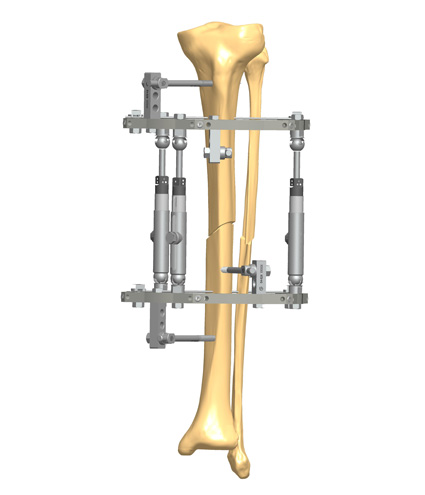
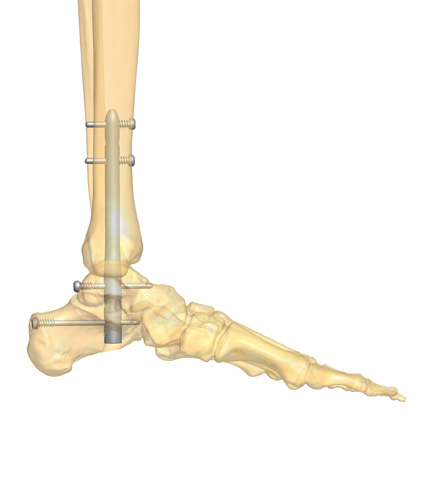
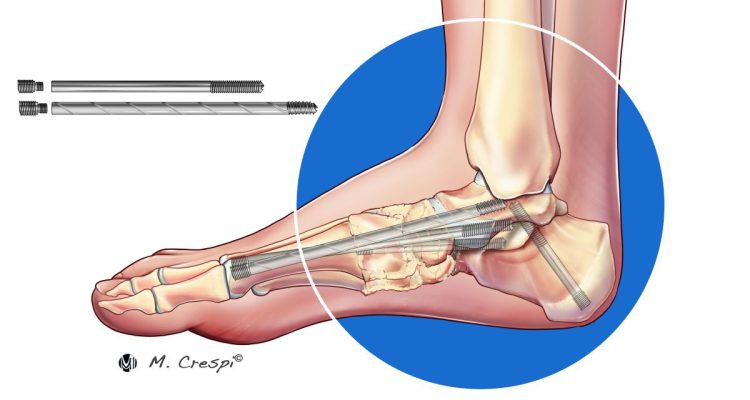
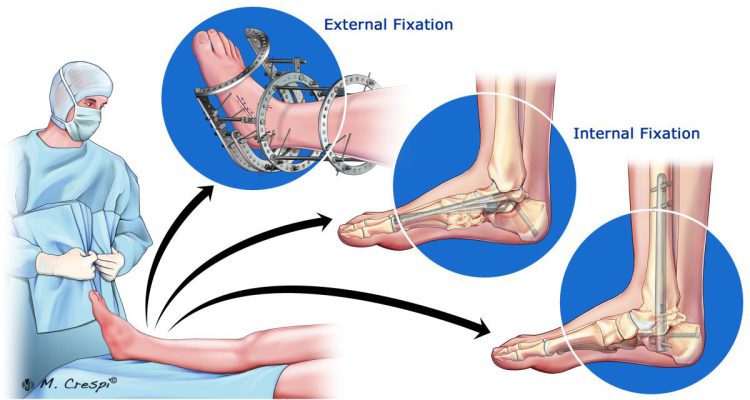
Charcot Foot Reconstruction Using Internal Fixation2023-12-12
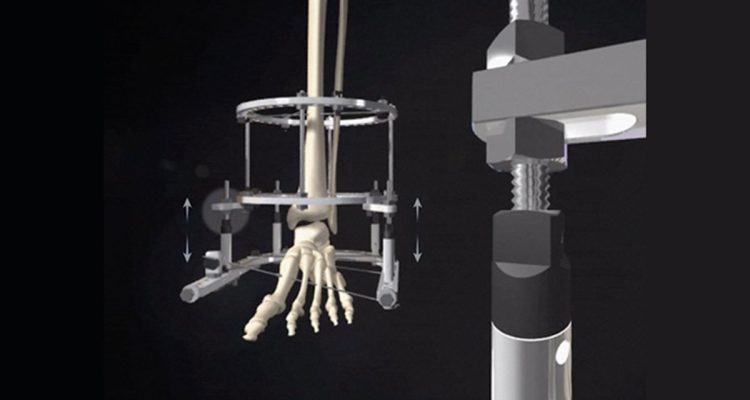
Appropriate timing for surgical intervention is a matter of controversy among specialists1. While in the past Charcot foot surgical reconstruction was mainly reserved to salvage the limb, today surgeons also perform operative corrections to ensure patients can use commercially available footwear instead of cumbersome orthoses1. Regardless, the main goal of Charcot foot surgery, independent of the fixation method, is to create a stable and plantigrade foot. This article will discuss different approaches for Charcot foot surgery with internal fixation, focusing on midfoot reconstruction.
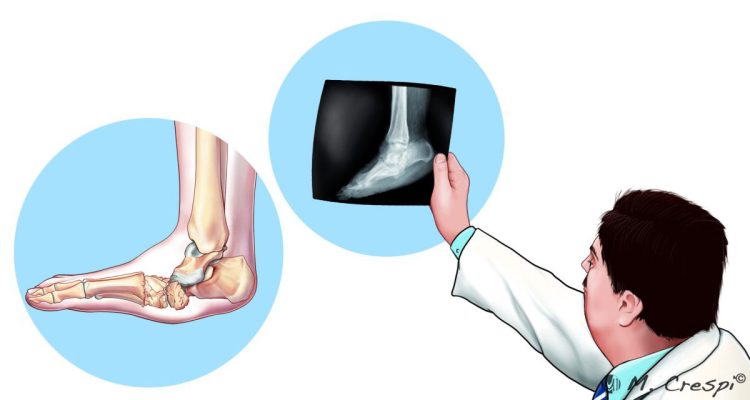
Expert Tips on How to Medically Diagnose Charcot Arthropathy2023-11-30
The diagnosis of Charcot neuroarthropathy of the foot and ankle can be challenging due to a lack of information in the patient's history, clinical assessment, imaging, and laboratory findings1. It is assumed that one in four cases of acute foot and ankle Charcot are undiagnosed or misdiagnosed1. However, correct diagnosis and effective treatment are crucial to avoid ulceration, worsening deformity, infection, or amputation1.
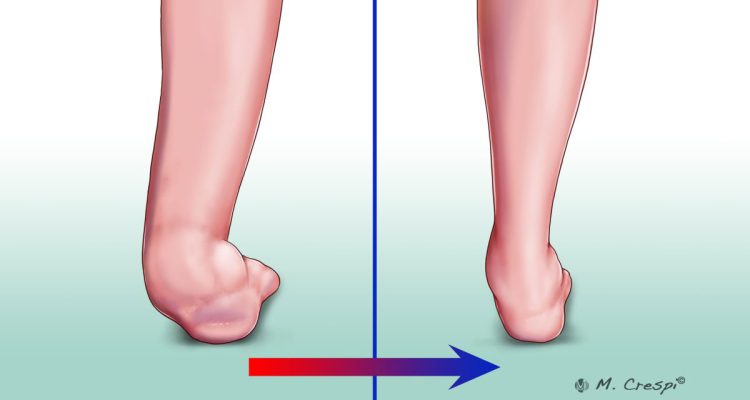
Charcot Arthropathy Symptoms and Initial Stage2023-11-21
Charcot arthropathy occurs in the presence of peripheral neuropathy and metabolic abnormalities. Today it is seen more commonly in patients with long-standing diabetes1,2. Its pathogenesis, although still largely unknown, involves several pro-inflammatory pathways, which stimulate osteoclastic activity3.
Medical Resources for Charcot Foot & Ankle Specialists2023-11-14
There is an overwhelming wealth of scientific literature available on Charcot foot. In this article, we gather and summarize some of the most interesting sources, including Charcot neuroarthropathy of the foot and ankle reviews, diabetic foot reviews, and diabetic foot care articles.
The Experts’ Definition of Diabetic Charcot Foot2023-11-14
Charcot foot is a progressive, devastating pathology defined by bone and joint changes that occur as a result of loss of sensation. Also called Charcot joint or neuropathic arthropathy, this condition is almost always associated with the vascular and neurological changes caused by poorly controlled diabetes1.
Charcot Surgical Reconstruction2023-11-14
Charcot foot, also called Charcot neuropathy, is a condition caused by a combination of peripheral neuropathy and vascular disorders that results in progressive joint damage and eventually foot instability1. If left untreated, the consequences for patients are devastating, with reduced quality of life, inability to weight-bear, and an increased risk of amputation2.
Surgical Approaches for Charcot Foot2023-11-14
Charcot neuroarthropathy is a rare, but devastating complication of diabetes1. Progressive destruction of the bones and joints of the foot cause deformities and thus alter foot biomechanics1. If not recognized nor treated properly, the disease can result in ulcer formation, infection, and progression of the disease with joint instability and bone destruction2,3. In the worst case, limb amputation is required4,5.
Tips for Timely Diagnosis of Charcot Foot and Ankle2022-01-17
It is known that around 9 per cent of patients with diabetic neuropathy and foot ulcers develop a Charcot foot and ankle. This pathology often goes unrecognized, particularly during the acute phase, until severe complications occur, such as an abnormal pressure distribution on the plantar fascia with bones weakened enough to fracture, followed by a marked foot and ankle deformation and, in the worst cases, by amputation. Thus, today, one of the most crucial questions is how to timely diagnose this condition.
Magnetic Resonance for Charcot Foot and Ankle Diagnosis2021-12-21
Charcot Foot and Ankle is a significant problem caused by peripheral neuropathy, with an estimated incidence of 0.3 to 7.5% in the diabetic population. This condition, which is also known as Charcot arthropathy, Charcot joint, or neuropathic arthropathy, affects the soft tissues, joints, and bones in the foot and ankle. If left untreated, it may lead to progressive foot deformity, ulceration, or osteomyelitis. In the most advanced stages, it may be necessary to resort to limb amputation.
Tips for the Prevention of Charcot Foot and Ankle2021-12-17
Charcot Foot and Ankle is a severe condition that, if left untreated, may lead to deformity, permanent disability, amputation or ultimately to the patient’s death. People with diabetic neuropathy are at high risk of developing Charcot Foot and Ankle, because of the decreased sensation and diminished ability to feel temperature, pain or trauma.
Computerized Tomography for Charcot Foot and Ankle Diagnosis2021-12-14
Charcot Foot and Ankle, also known as Charcot arthropathy or Charcot joint, is a condition caused by peripheral neuropathy, leading to the progressive degeneration and destruction of the soft tissue, joint, and bone. In modern society, the most common cause for this neuropathic neuropathy is diabetes mellitus, with long-term diabetic patients having an increased risk of developing the condition.
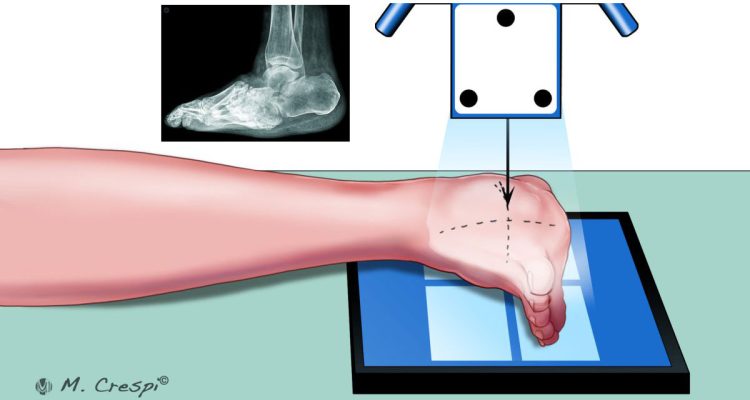
Radiography for Charcot Foot and Ankle Diagnosis2021-12-07
Charcot Foot and Ankle, also known as Charcot arthropathy, neuropathic arthropathy or Charcot joint, is a progressive condition that affects the bones, joints and soft tissue of the foot and ankle. It is caused by peripheral neuropathy. Today, diabetes is the most common cause for developing Charcot Foot and Ankle.
Charcot Foot and Ankle Causes: Where the Pathology Starts2021-11-25
Charcot Foot and Ankle, also known as Charcot arthropathy, is a progressive, inflammatory condition that affects the bones, joints, and soft tissues in the feet of people with peripheral neuropathy. If left untreated, Charcot of the foot and ankle leads to severe deformity, ulceration, and – worst-case scenario – to limb amputation.
Charcot Foot and Ankle: Definition and Classification2021-11-12
Charcot Neuroarthropathy, also called Charcot Foot and Ankle, is a progressive and inflammatory condition that weakens the soft tissues, bones, and joints of the foot and ankle. This complex and challenging type of neuropathic arthropathy is commonly linked to diabetes. If left untreated, it can lead to devastating consequences, such as deformity, ulceration, and infection. In the worst-case scenario, it may result in limb amputation.
The Surgical Approach to the Charcot Foot and Ankle Treatment2021-05-24
Charcot Foot and Ankle is a complex, challenging and sometimes devastating inflammatory foot disease which causes loss of sensation, weakening of the bones and collapse of the weight bearing joints. Most often due to diabetes and underlying neuropathic arthropathy, it needs a multidisciplinary team approach in order to treat it properly and prevent amputation.
What Is Arthrodesis (Joint Fusion)?2021-05-06
Arthrodesis may be defined as the surgical immobilization of a joint by fusion of the bones. It is commonly referred to as joint fusion, also known as artificial ankylosis or syndesis. It can be performed in several parts of the body, and it is indicated in the presence of painful joints, often due to arthritis or osteoarthritis, with highly compromised mobility.