There is an overwhelming wealth of scientific literature available on Charcot foot. In this article, we gather and summarize some of the most interesting sources, including Charcot neuroarthropathy of the foot and ankle reviews, diabetic foot reviews, and diabetic foot care articles.
Articles on the Medical Condition
Drs. Lee C. Rogers and Robert G. Frykberg have authored many scientific articles and textbook chapters with a focus on Charcot foot and diabetic foot problems. In a paper published in 2013, titled “The Charcot Foot,” they review the epidemiology of the condition, highlighting that although much about its pathophysiology is still unknown, most experts agree that it is the combination of existing neuropathy with trauma – even a minor one – that kindles the syndrome.1 The first stage is then accompanied by inflammation, releasing cytokines including tumor necrosis factor-alpha and interleukin-1-beta. These cytokines will then trigger a metabolic pathway in which osteoclasts’ maturation will be stimulated and osteoblasts’ function will be reduced, ultimately leading to bone destruction. The authors continue their article by reviewing forms of diagnosis and the classification of Charcot foot, noting that more complicated cases of Charcot foot (with deformity, ulceration, and osteomyelitis) that have a more proximal location (in the rearfoot and/or ankle) are associated with an increased risk of amputation.1
These two specialists were also part of an international task force of experts that were brought together by the American Diabetes Association and the American Podiatric Medical Association in January 2011 to summarize the available evidence on the pathophysiology, natural history, presentations, and treatment recommendations for “The Charcot Foot in Diabetes”.2 The scientific article that resulted from the specialists’ review of the available literature is a condensed, pertinent text with the most distinguishing features of the condition, its pathogenesis, diagnosis, and treatment recommendations. The article also includes a decision algorithm for a basic approach to a suspected Charcot foot case.2 The authors call attention to the fact that osteomyelitis can be difficult to distinguish from Charcot foot on plain radiographs or nuclear imaging. In such cases, magnetic resonance imaging (MRI) can be the test of choice to evaluate the complicated foot in patients with diabetes.2 Regarding treatment options, the experts agree that off-loading is the most important initial recommendation, but recognize that surgery can be helpful in early stages including acute fractures or in later stages when off-loading is no longer effective.2
Other useful resources for the clinicians who would like to have an overview of the condition include:
- The Essentials of Charcot Neuroarthropathy3, edited by Claude Pierre-Jerome, covers the epidemiology, biomechanics, pathophysiology, socioeconomic impacts, radiological findings, and differential diagnosis of Charcot foot in diabetic patients, with an emphasis on MRI.
- Diabetes Mellitus: An Overview in Relationship to Charcot Neuroarthropathy4, authored by Lindsey R. Hjelm, describes the existence of Charcot foot in the context of diabetes mellitus, both of type 1 and type 2. The author highlights that diabetic patients are particularly vulnerable to progressive disease, due to increased bone fragility, although there is also some evidence of the protective effects of insulin and metformin on bone quality.4
- Etiology, Epidemiology, and Outcomes of Managing Charcot Arthropathy5, by Thomas Hester and Venu Kavarthapu, who focused on the desired outcomes of managing Charcot foot: limb salvage, structural stability of the foot and ankle, eradication of any existing infection, ulcer prevention, and restoration of a plantigrade foot.
Articles on Treatment
Many articles that provide an overview of Charcot foot also include sections on treatment, since this is an essential component to improve outcomes in the patients who suffer from it. If the condition is left untreated, its natural history is one of progressive foot deformity, often requiring amputation in later stages or when there is concomitant infection.6 The main objective of treatment is to achieve a stable and pain-free plantigrade foot, ideally allowing patients to use commercially available shoes instead of custom-made orthotics.7,8
Some articles, like the one authored by Felix W.A. Waibel and Thomas Böni, have a specific focus on conservative management. In their article, titled “Nonoperative Treatment of Charcot Neuro-osteoarthropathy,” the authors state that whenever there is a suspicion of active Charcot foot, there should be immediate off-loading and a decrease in physical activity to prevent progression.9 If the patient is unable to cope with the off-loading device, short hospitalization and instruction physiotherapy can be considered to ensure adherence to treatment. After the active phase of Charcot foot, when off-loading with either irremovable or removable total contact casts are recommended, patients are advised to wear orthopedic footwear to reduce pressure while walking, thus preventing ulcer formation and bone injury, which would lead to Charcot foot reactivation.9
Surgical treatment is indicated whenever:
- There is severe deformity with an open wound and osteomyelitis9
- There is severe deformity with an open wound refractory to off-loading9
- There is severe midfoot or hindfoot deformity with instability9
- There is severe deformity with recurrent ulcers despite initial healing with off-loading9
- Conservative management is not enough to avoid ulcer formation7
- There is impending ulcer formation associated with severe dislocation7
- There is instability and increased plantar pressure7
Broadly speaking, the available surgical treatments for patients with Charcot neuroarthropathy can be grouped into 3 types of procedures: those aiming to correct soft tissue imbalances, exostectomies, and reconstruction.7 The appropriate surgical route is chosen after careful consideration of each patient, since each case is different and there are multiple factors that impact the results.7,10
The topic of “Surgical Optimization for Charcot Patients” is addressed by Kelsey J. Millonig, DPM and Rachel Gerber, DPM in a recent article. There is no clear consensus on the best treatment approach. Although there is a significant risk for amputation with or without reconstructive treatment for Charcot foot, there are modifiable risk factors associated with Charcot reconstruction in the preoperative stage. The authors provide a few pre-surgical instructions to address these risk factors, including:
- Encourage well-controlled glucose levels in patients with diabetes
- Evaluate the existence of peripheral vascular disease beyond clinical examination findings
- Promote tobacco cessation no later than 8 weeks before surgery
- Evaluate renal function, paying particular attention to patients with end-stage renal disease and chronic kidney disease
- Assess the presence of obesity, hypertension, edema, the patient’s metabolic profile, and the presence of infection11
These factors can impact the success of surgical reconstruction in Charcot foot beyond the surgical technique or devices used, and it is therefore essential that surgeons consider them carefully.11
For instance, exostectomies can be used to manage recurrent and/or recalcitrant ulcers, for which conservative treatment has failed.7,8 In these cases, the excision of bony protuberances can promote ulcer healing and reduce their recurrence, especially in the mid- and hindfoot.8 However, this is an intervention in which a balance needs to be found between enough and excessive bone resection, since insufficient bone excision will not prevent ulcer recurrence, while too much can result in wound healing complications and foot instability.7,12
“Surgical procedures are ultimately chosen depending on each clinical scenario,” say Alan C. Stuto and John J. Stapleton in their article, “Surgical Considerations for the Acute and Chronic Charcot Neuroarthropathy of the Foot and Ankle.”13 The authors note that the goals of surgery will depend on the characteristics and stage of the disease:
- In the acute stage, the goal is to provide stabilization. This can be achieved with gradual deformity correction and delayed osseous reconstruction or with a one-stage procedure where both correction and reconstruction are addressed. It is worth noting that surgical treatment in the acute stage is the exception and not the rule due to the high failure rate.
- After the acute phase subsides, the focus of surgical management is on deformity correction.
Depending on the specific goals of the surgery, the deformity correction can be done through osteotomies and/or joint arthrodesis with internal and/or external fixation.13 The type of fixation depends mostly on the surgeon’s preference and familiarity, but some general principles can be applied. If there is ulceration or infection, a staged approach with tissue debridement and initial application of an external fixator is preferred; meanwhile for definitive fixation, both internal or external fixators can be used.7 More details on the types of fixation are provided in the section below.
Although the outcomes of a surgically repaired Charcot foot are not always easy to predict, surgical reconstruction has been associated with better quality of life in patients, compared with life-long bracing or amputation.14
Articles on Fixation Devices
The renewed interest in the surgical reconstruction of Charcot foot deformities has led to the publication of several scientific articles on the subject. In a recent systematic review by Joon Ha and colleagues, the authors analyzed the outcomes of Charcot foot reconstruction, concluding that surgical management can offer limb salvage to a select population.15
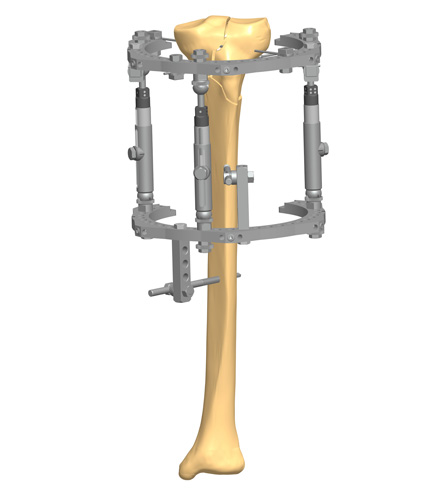
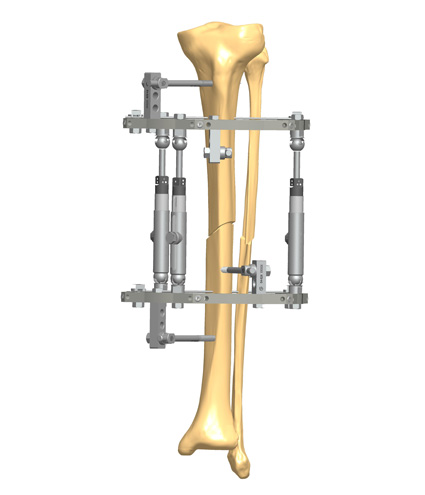
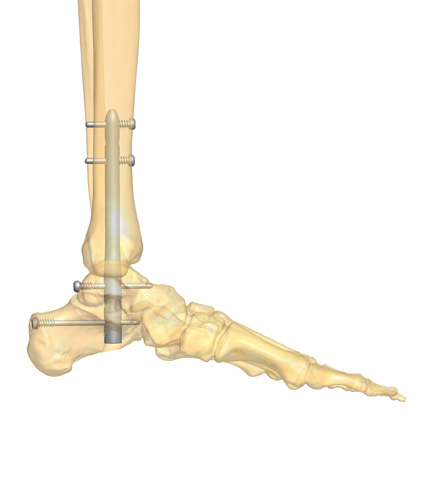
Both internal and external fixation devices can be used for the surgical reconstruction of the Charcot foot. Circular or hexapod external fixation is preferred when there is infection, poor bone stock, or the soft tissue envelope is already compromised (e.g., from ulceration).13,16 Internal fixation devices can be:
- Plates and screws
- Beams, screws, or bolts
- Intramedullary nails
Many times, the reconstruction of a Charcot foot will require several different internal fixation devices, or even a combination of external and internal devices, according to the level and location of the deformity.16
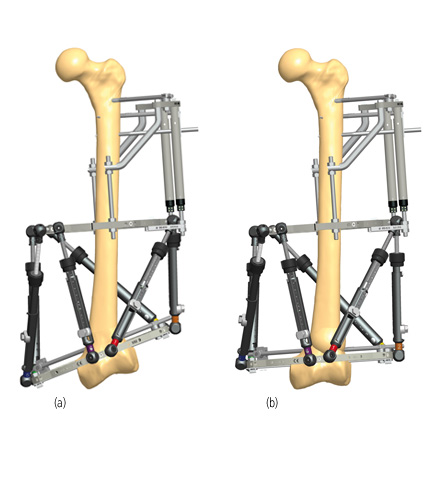
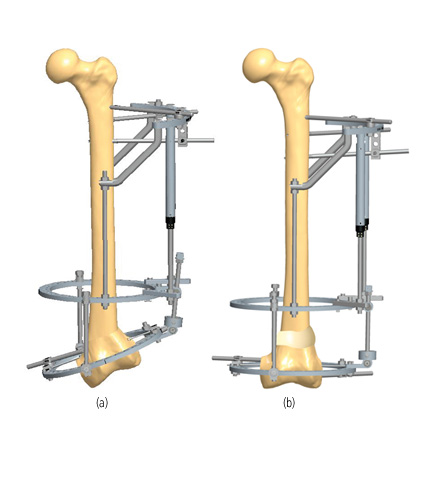
External fixation can be a powerful and versatile tool in the management of Charcot foot, states Dr. Byron Hutchinson in his article “Circular Fixation in Charcot,” where he also discusses aspects of frame application and biomechanics.17
In a comprehensive article titled “The Use of Hexapod External Fixation in the Management of Charcot Foot and Ankle Deformities,” Dr. Guido LaPorta and colleagues provide useful advice for the use of a 2-stage computer hexapod-assisted technique to address midfoot Charcot and ankle-hindfoot deformities with the goal of restoring function and decreasing the risk of amputation secondary to ulceration and infection.18In a systematic review of outcomes following intramedullary fixation for midfoot Charcot foot, Wukich and colleagues found that the use of intramedullary screws (solid or cannulated), also referred to as bolts or beams, that are inserted into cancellous Charcot bone or that cross large bone voids can delay osseous incorporation.19 They also note that in the cases where bolts were used, migration was more common than breakage, which may be a result of implant design due to the lack of medial column stability. In an effort to assess the construct rigidity and strength of beaming and plantar plating of the medial column, Simonik et al performed a biomechanical study to compare the construct rigidity and strength of beaming and plantar plating, concluding that while both implant types were similar in terms of stiffness, beams were able to withstand significantly more load before failure occurred.20 Another aspect to consider is that the use of plates and screws to reconstruct midfoot deformities requires an adequate soft tissue envelope and is associated with a high failure rate.13,21
To address these limitations, surgeons developed ‘super constructs,’ a method where some of the normal principles of orthopedic techniques are abandoned to improve stability and reduce the likelihood of failure of the procedure.22 A ‘super construct’ is defined by four factors:
- Application of hardware beyond the injury area, including nearby joints
- Bone resection to allow for adequate reduction without compromise of the soft tissue envelope
- Use of the strongest device(s) that can be tolerated by the soft tissue envelope
- Application of the devices in a position that maximizes mechanical function
‘Super constructs’ can be achieved with the use of large intramedullary screws or with other devices.21 The mechanics, technique and hardware considerations are addressed in the article “Beaming the Charcot Foot” by Drs. William Grant and Lisa Grant-McDonald.21
The use of super construct reconstruction principles was applied by Frøkjær in a series of 20 Charcot foot patients with midfoot collapse, 2 of whom presented with an ulcer and osteomyelitis.23 A two-staged approach was used, with preoperative off-loading in all cases and temporary external fixation in the 2 infection cases. After the initial off-loading stage, patients had definitive reconstruction with screws and plates. The author reported promising outcomes, with 95% of patients achieving an ulcer-free, stable, and plantigrade foot after a mean follow-up time of 24 months, despite the high rate (40%) of postoperative wound healing problems.23
Charcot neuroarthropathy in both the hindfoot and the midfoot results in complex deformities, which have a high risk of ulceration, infection, and limb amputation if uncorrected.24 Although technically demanding, reconstruction of hindfoot and midfoot Charcot deformities can be carried out with the use of internal fixation. In a recent article titled “Combined Charcot hindfoot and midfoot reconstruction using internal fixation method – surgical technique and single surgeon series,” Kavarthapu and colleagues present the surgical technique and outcomes of deformity correction and stabilization using a hindfoot nail, midfoot beams, and locking plates.24 The authors performed 35 reconstruction procedures in 34 patients with limb-threatening deformity due to Charcot neuroarthropathy, showing that the proposed technique provided functional limb salvage in most cases, with an acceptable level of complications.
Patients with a hindfoot or ankle Charcot neuroarthropathy deformity can be managed with arthrodesis.25 In a thorough review titled “Tibial Lengthening and Intramedullary Nail Fixation for Hindfoot Charcot Neuroarthropathy,” Drs. Kelsey J. Millonig and Noman A. Siddiqui explore the outcomes of tibiocalcaneal arthrodesis with distal tibial lengthening in patients with neuropathy and provide some guiding principles of external and internal fixation in this patient population. They highlight that intramedullary nailing reduces the duration of external fixation and protects the regenerate during fixation, which is relevant for neuropathic patients. The combined use of internal and external fixation was also reported by El-Mowafi et al. in their article “Hybrid Fixation for Ankle Fusion in Diabetic Charcot Arthropathy.” The authors note that the poor bone quality often hinders ankle fusion in patients with type 3a (Brodsky) Charcot neuropathy. Nonetheless, they were able to obtain successful ankle fusions in their patients by combining an intramedullary nail that was locked only at the proximal end and a ring external fixator, avoiding amputation in all patients of their complex cohort.26
Another way to reduce the complication rate in reconstruction procedures is to use a minimally invasive surgical (MIS) approach. This was reported by Mateen et al. in the article “Comparison of Minimally Invasive and Open Approaches for Midfoot Charcot Neuroarthropathy Reconstruction,” where the authors compared outcomes in 17 patients who underwent midfoot reconstruction with a MIS approach versus 17 patients who underwent reconstruction with a traditional approach. They found that wound problems occurred only with the traditional (open) approach. Although MIS approach was not without complications, such as pin site infection, the authors concluded that this method offered similar outcomes to the more traditional approach.27
In the article “Charcot foot reconstruction outcomes: A systematic review,” a total of 1116 feet in 1089 patients were included. From that cohort, 346 patients were managed with external fixation, 726 with internal fixation, and 44 with a combination of internal plus external fixation. The authors could not find a preferential method of fixation, since all methods resulted in high fusion and low amputation rates, but also high complication rates.15 This is a reflection not only of the complexity involved in Charcot foot reconstruction, but also of the challenges of managing such conditions in highly morbid patients.
Some technological advancements have been made to improve the chance of success in surgical interventions for Charcot foot patients, including the use of computer-assisted deformity correction. Wrotslavsky and colleagues published an article in which they report on the use of computer-assisted external fixation to gradually and accurately correct the Meary and calcaneal inclination angles in a series of 18 patients with Charcot foot, 13 of whom had also ulceration. The outcomes were good, with radiographic parameters within acceptable limits and complete ulcer healing observed in all patients. The authors concluded that computer-assisted deformity correction is safe and adequately prepares the foot for the second stage, the implantation of internal fixation.12
Articles on Prevention of Infections
Infection is a common problem for patients with Charcot neuroarthropathy, either in the form of ulcers or as a result of treatment with external fixators. Pin site infection in the place where K-wires and metal pins pierce the skin are so common that some consider it to be an inevitable complication of treatment with external fixators. There are notable comorbidities associated with pin site infections including diabetes and vascular diseases, conditions also present in many Charcot patients.28,29
Despite numerous studies investigating the prevention of pin site infections, there has been no consensus to date on the best regime to avoid this complication. Although these infections may be self-contained and relatively manageable, there are cases where the infection spreads to adjacent tissues and even bone, becoming a much bigger problem. In addition, there is evidence that pin site infections increase the cost of treatments, delay treatment completion, and aggravate patient burden.30,31
One intervention that has recently demonstrated effective results in both retrospective and prospective case series is the use of a microbicidal liquid polymer. After cleaning the pin sites with a soft toothbrush or gauze per usual standard of care, the liquid polymer is applied to each pin site, where microorganisms (bacteria, fungi, and viruses) are immediately eradicated upon contact. As the solvent evaporates, a thin elastomeric film is formed that has occlusive properties to protect the pin site against entry of water, microorganisms, and dirt. Its flexibility makes it suitable to apply to all skin areas, especially where there are creases or a need for extensive flexing and bending such as in the foot.28,29
Conclusion
Charcot foot is a complex problem, which arises from peripheral neuropathy and is today more prevalent among patients with diabetes.2 Surgical reconstruction is a challenging procedure, with a high complication rate. Nonetheless, it is indicated for some patients or in cases of advanced disease, for whom it can be an alternative to limb amputation and provide better quality of life.15
There are several fixation devices available, both internal and external, and it is up to the surgeon to take into consideration the patient characteristics and condition features before deciding on the best approach for each Charcot foot case.
To help better understand the array of surgical approaches available to treat Charcot patients, a series of Charcot Reconstruction Case Reports has been created and is available to subscribers and registered users.

References
1. Rogers LC, Frykberg RG. The Charcot Foot. Medical Clinics of North America. 2013/09/01/ 2013;97(5):847-856. doi:https://doi.org/10.1016/j.mcna.2013.04.003
2. Rogers LC, Frykberg RG, Armstrong DG, et al. The Charcot Foot in Diabetes. Journal of the American Podiatric Medical Association. 01 Sep. 2011 2011;101(5):437-446. doi:10.7547/1010437
3. Pierre-Jerome C. The essentials of charcot neuroarthropathy: biomechanics, pathophysiology, and MRI findings. Elsevier; 2022.
4. Hjelm LR. Diabetes Mellitus: An Overview in Relationship to Charcot Neuroarthropathy. Clinics in Podiatric Medicine and Surgery. 2022/10/01/ 2022;39(4):535-542. doi:https://doi.org/10.1016/j.cpm.2022.05.001
5. Hester T, Kavarthapu V. Etiology, Epidemiology, and Outcomes of Managing Charcot Arthropathy. Foot and Ankle Clinics. 2022/09/01/ 2022;27(3):583-594. doi:https://doi.org/10.1016/j.fcl.2022.03.002
6. Dardari D. An overview of Charcot’s neuroarthropathy. J Clin Transl Endocrinol. Dec 2020;22:100239. doi:10.1016/j.jcte.2020.100239
7. Khan O, Kavarthapu M, Edmonds M, Kavarthapu V. Surgical management of Charcot foot – The advancements over the past decade. Journal of Clinical Orthopaedics & Trauma. 2023;47doi:10.1016/j.jcot.2023.102317
8. Lowery NJ, Woods JB, Armstrong DG, Wukich DK. Surgical Management of Charcot Neuroarthropathy of the Foot and Ankle: A Systematic Review. Foot & Ankle International. 2012;33(2):113-121. doi:10.3113/fai.2012.0113
9. Waibel FWA, Böni T. Nonoperative Treatment of Charcot Neuro-osteoarthropathy. Foot and Ankle Clinics. 2022/09/01/ 2022;27(3):595-616. doi:https://doi.org/10.1016/j.fcl.2022.05.002
10. Bajuri MY, Ong SL, Das S, Mohamed IN. Charcot Neuroarthropathy: Current Surgical Management and Update. A Systematic Review. Front Surg. 2022;9:820826. doi:10.3389/fsurg.2022.820826
11. Millonig KJ, Gerber R. Surgical Optimization for Charcot Patients. Clinics in Podiatric Medicine and Surgery. 2022/10/01/ 2022;39(4):595-604. doi:https://doi.org/10.1016/j.cpm.2022.05.006
12. Wrotslavsky P, Kriger SJ, Hammer-Nahman SM, Kwok JG. Computer-Assisted Gradual Correction of Charcot Foot Deformities: An In-Depth Evaluation of Stage One of a Planned Two-Stage Approach to Charcot Reconstruction. The Journal of Foot and Ankle Surgery. 2020;59(4):841-848. doi:10.1053/j.jfas.2019.06.008
13. Stuto AC, Stapleton JJ. Surgical Considerations for the Acute and Chronic Charcot Neuroarthropathy of the Foot and Ankle. Clinics in Podiatric Medicine and Surgery. 2022/04/01/ 2022;39(2):331-341. doi:https://doi.org/10.1016/j.cpm.2021.11.005
14. Albright RH, Joseph RM, Wukich DK, Armstrong DG, Fleischer AE. Is Reconstruction of Unstable Midfoot Charcot Neuroarthropathy Cost Effective from a US Payer’s Perspective? Clinical Orthopaedics and Related Research®. 2020;478(12)
15. Ha J, Hester T, Foley R, et al. Charcot foot reconstruction outcomes: A systematic review. J Clin Orthop Trauma. May-Jun 2020;11(3):357-368. doi:10.1016/j.jcot.2020.03.025
16. Abyar E, McKissack H, Johnson MD. Chapter 19 – The surgical management of the Charcot foot: physical examination of the foot prior to surgery, indications and criteria for amputation, and surgical techniques. In: Pierre-Jerome C, ed. The Essentials of Charcot Neuroarthropathy. Elsevier; 2022:441-448.
17. Hutchinson B. Circular Fixation in Charcot. Clinics in Podiatric Medicine and Surgery. 2022/10/01/ 2022;39(4):643-658. doi:https://doi.org/10.1016/j.cpm.2022.05.008
18. LaPorta GA, Begum M, Guzelak S, D’Andelet A. The Use of Hexapod External Fixation in the Management of Charcot Foot and Ankle Deformities. Clinics in Podiatric Medicine and Surgery. 2022/10/01/ 2022;39(4):629-642. doi:https://doi.org/10.1016/j.cpm.2022.05.010
19. Wukich DK, Liu GT, Johnson MJ, et al. A Systematic Review of Intramedullary Fixation in Midfoot Charcot Neuroarthropathy. The Journal of Foot and Ankle Surgery. 2022/11/01/ 2022;61(6):1334-1340. doi:https://doi.org/10.1053/j.jfas.2022.04.009
20. Simonik MM, Wilczek J, LaPorta G, Willing R. Biomechanical Comparison of Intramedullary Beaming and Plantar Plating Methods for Stabilizing the Medial Column of the Foot: An In Vitro Study. The Journal of Foot and Ankle Surgery. 2018/11/01/ 2018;57(6):1073-1079. doi:https://doi.org/10.1053/j.jfas.2018.03.043
21. Grant W, Grant-McDonald L. Beaming the Charcot Foot. Clinics in Podiatric Medicine and Surgery. 2022/10/01/ 2022;39(4):605-627. doi:https://doi.org/10.1016/j.cpm.2022.05.007
22. Sammarco VJ. Superconstructs in the Treatment of Charcot Foot Deformity: Plantar Plating, Locked Plating, and Axial Screw Fixation. Foot and Ankle Clinics. 2009/09/01/ 2009;14(3):393-407. doi:https://doi.org/10.1016/j.fcl.2009.04.004
23. Frøkjær J. Surgical treatment of midfoot charcot neuroarthropathy review of literature and our results after superconstruct reconstruction of midfoot charcot neuroarthropathy. Journal of Clinical Orthopaedics & Trauma. 2021;17:59-64. doi:10.1016/j.jcot.2021.02.003
24. Kavarthapu V, Guduri V, Hester T. Combined Charcot hindfoot and midfoot reconstruction using internal fixation method—surgical technique and single surgeon series. Annals of Joint. 2023;8
25. Millonig KJ, Siddiqui NA. Tibial Lengthening and Intramedullary Nail Fixation for Hindfoot Charcot Neuroarthropathy. Clinics in Podiatric Medicine and Surgery. 2022/10/01/ 2022;39(4):659-673. doi:https://doi.org/10.1016/j.cpm.2022.05.011
26. El-Mowafi H, Abulsaad M, Kandil Y, El-Hawary A, Ali S. Hybrid Fixation for Ankle Fusion in Diabetic Charcot Arthropathy. Foot & Ankle International. 2018;39(1):93-98. doi:10.1177/1071100717735074
27. Mateen S, Thomas MA, Siddiqui NA. Comparison of Minimally Invasive and Open Approaches for Midfoot Charcot Neuroarthropathy Reconstruction. The Journal of Foot and Ankle Surgery. 2023;62(6):986-990. doi:10.1053/j.jfas.2023.08.001
28. Pema S. Retrospective Evaluation of Microbicidal Polymer Dressing for Reduction of Infection Following Post Deformity Correction Surgery. J Drugs Dermatol. Dec 1 2018;17(12):1322-1324.
29. Pema S. An evaluation of the use of a novel microbicidal liquid polymer for the reduction of pin-tract infection in external fixation procedures for deformity correction and traumatic provisional fixation. Clin Microbiol Infect Dis. 2020 2020;5(3)doi:10.15761/CMID.1000177
30. Kazmers NH, Fragomen AT, Rozbruch SR. Prevention of pin site infection in external fixation: a review of the literature. Strategies Trauma Limb Reconstr. Aug 2016;11(2):75-85. doi:10.1007/s11751-016-0256-4
31. Lethaby A, Temple J, Santy‐Tomlinson J. Pin site care for preventing infections associated with external bone fixators and pins. Cochrane Database of Systematic Reviews. 2013;(12)doi:10.1002/14651858.CD004551.pub3