Charcot neuroarthropathy of the ankle is an especially challenging condition that often leads to instability and destruction of the joint with significant morbidity requiring an amputation in many instances1-3. According to Brodsky et al., the ankle is affected in 9% of patients with Charcot neuroarthropathy, whereas the hindfoot is involved in 30-35%3. The overall goal of Charcot ankle reconstruction is to achieve a painless, plantigrade and stable foot, and thus avoid ulceration with subsequent infection1,2. However, this procedure is also associated with a high complication rate1,2.
Anatomy and Biomechanics of Charcot Ankle
The ankle joint is a modified synovial hinge joint that is formed by the articulations of the talus, tibia and fibula (Figure 1)3. The congruency of the bone and ligaments of the ankle creates a high level of stability.3 This is important as the ankle joint bears about five times the body weight in the stance phase during normal gait, which increases to 13 times the body weight during activities such as running3. In contrast to midfoot deformities, Charcot neuroarthropathy at the hindfoot and ankle level is often multiplanar and can be more challenging to treat3. Alteration of the biomechanics and proprioception of the involved ankle often results in gait changes, whereas, malalignment of the Charcot limb makes it more prone to ulceration due to altered pressure distribution and limited soft tissue coverage3. These changes are often associated with limb shortening due to bone collapse caused by avascular necrosis or fractures3.
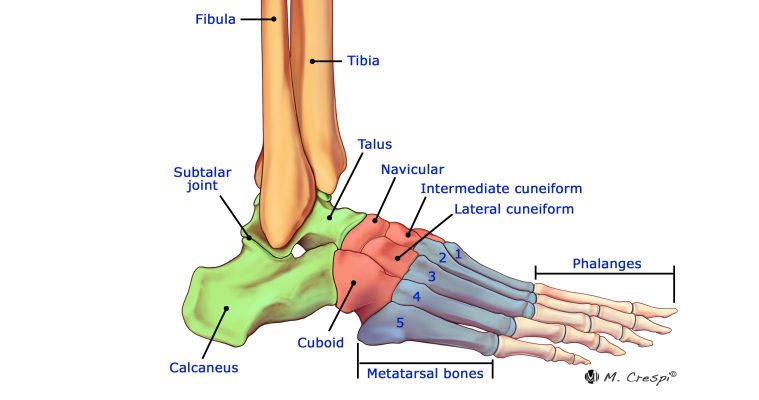
Source: https://www.csog.net/the-basics-of-ankle-anatomy-and-foot-anatomy/
Tibiotalocalcaneal Arthrodesis
Surgical reconstruction of the Charcot hindfoot and ankle is preferred over conservative techniques, since malalignment and bony prominences often make the limb not suitable for bracing4. Tibiotalocalcaneal arthrodesis aims to inhibit the ankle joint motion and is frequently performed to address Charcot in the hindfoot or ankle, but also in cases of severe osteoarthritis, avascular necrosis of the talus, or in the revision of failed arthroplasty5. The combination of poor structural bone quality in Charcot patients and the biomechanical challenge of a long moment arm applied during stance phase make stable and secure fixation a challenge6.
Intramedullary Nailing
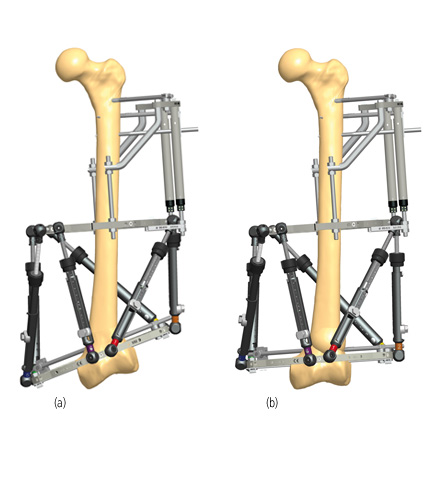
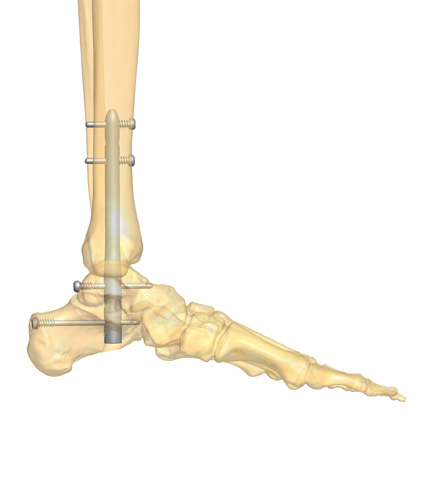
In patients with Charcot neuroarthropathy, retrograde locked intramedullary nailing is considered one of the best options for tibiotalocalcaneal arthrodesis (Figure 2), especially in patients at high risk for postoperative complications2,6, as the nail can be inserted via small incisions with minimal soft tissue dissection2. The load-sharing properties of tibiotalocalcaneal nails provide compression across the ankle and talocalcaneal joints and thus allow early weightbearing2. In general, intramedullary nails were shown to provide higher stability for axial compression and torsion when compared to external fixators3. However, in more complex deformities hybrid fixation should be considered as it is associated with a higher rate of limb salvage and low soft tissue irritation rates3.

The most common complications of tibiotalocalcaneal arthrodesis are local deep infection, perioperative fracture and subsidence of the components, neurologic affection, delayed union or complete nonunion5. Reoperations are more frequent as well when a talectomy has been performed6.
Lisa Grant-McDonald (DPM, Doctors Grant Foot & Ankle, Virginia Beach) explains her approach for tibiotalocalcaneal arthrodesis: “I try to salvage the talus whenever it’s possible. However, when the talus is necrotic, all dead bone must be removed. In this situation, a talus implant should be considered to hold the hindfoot nail appropriately and avoid windshield wiper effect.”
As an alternative to talus implants, Stephanie Oexeman (DPM, Oexeman Foot & Ankle, Chicago) recommends: “Tibiocalcaneal arthrodesis with distal lengthening is my preferred technique when the talus isn’t salvageable. The benefit of distal lengthening is that it can enhance the vascularity of the arthrodesis site.”
Daniel Scott (Medical University of South Carolina (MUSC) Orthopaedics, Charleston) offers another possible solution: “Consider the fibula as an autograft when salvage of the talus is not feasible. Some shortening can be accepted in these cases.”
Alternatives to nailing for tibiotalocalcaneal arthrodesis are internal fixation with screws and plates, external fixation alone, or the combination of internal and external fixation5. However, screw fixation and external fixation alone are associated with low union rates5.
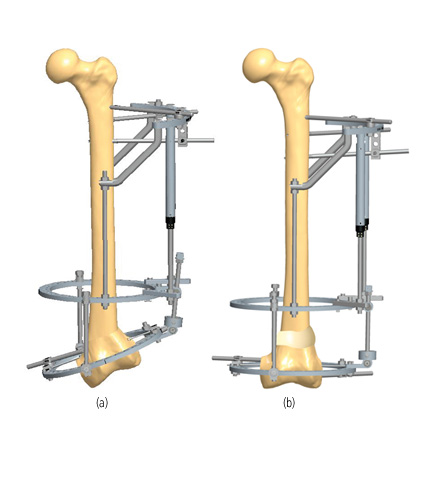
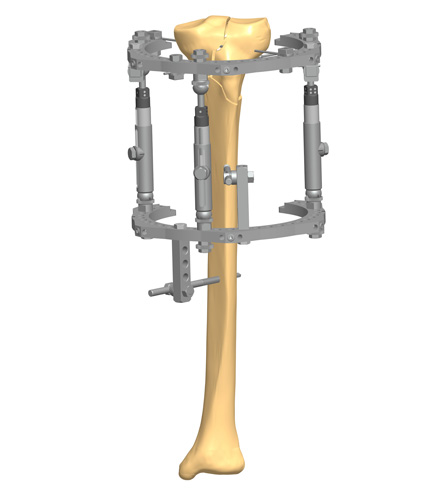
Circular Fixation and Hybrid Constructs
Tibiotalocalcaneal arthrodesis with a circular fixator has the benefit of being less invasive, preserving the blood supply, and allowing axial micromotion of bone fragments during weightbearing3. In addition, adaptations in the frame components can be used for staged deformity corrections without soft tissue tensioning3. Therefore, circular fixators are often considered in patients presenting with late deformity, soft tissue compromise and infection, which are contraindications to primary internal fixation7. The possibility for gradual corrections makes them an optimal solution to address severe Charcot deformities in single or two-stage approaches7. At least two fixation points per ring are recommended and stability can be increased by adding additional fixation elements per ring7.
The use of hybrid constructs with a circular fixator and a form of internal fixation is frequently cited and is associated with high rates of limb salvage and bone union3,8. The added stability by circular fixation can be beneficial in patients who are at high risk for complications or require extended arthrodesis8. It is important that the wires and pins of the circular fixator have no contact with the internal fixation to avoid deep infections7.
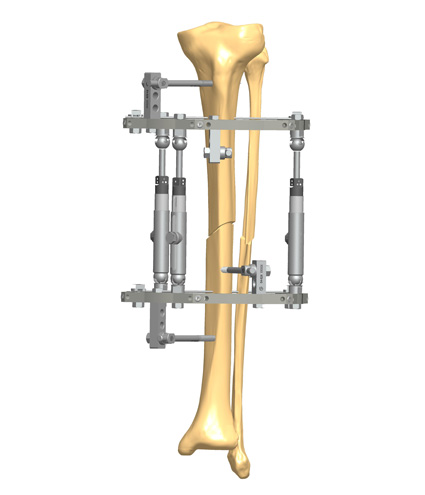
Plates
Although less frequently used than intramedullary nails or external fixators, arthrodesis with a plate via the posterior approach is an alternative reconstruction option for Charcot ankle9. Of course, the plate insertion requires a more invasive approach via a longitudinal incision on the lateral border of the Achilles’ tendon, posterior capsular resection, removal of the cartilage and fibrous tissues, and resection or restoration of the talus9. Locking plates are frequently used because they significantly enhance the structural stability of plates and screws, are highly resistant to shear and pull out force, and preserve the periosteal blood supply since they have no direct pressure to the bone10. In certain patients, tibiotalocalcaneal arthrodesis with a locking plate is a safe method with relatively short operative and fluoroscopy time10.
Conclusion
Despite being a technically demanding procedure, tibiotalocalcaneal arthrodesis is considered safe and effective to surgically manage Charcot neuropathy in the hindfoot and ankle5. However, major complications might occur in diabetic patients, even in the presence of bone union5. Therefore, achieving successful clinical outcomes also depends on thorough preoperative planning and the collaboration of a multidisciplinary team7.
Further Reading
For more information about Charcot foot reconstruction of the ankle, we have compiled a case report highlighting an example of Charcot ankle reconstruction available here.

References
1. Wang G, Lin J, Zhang H, Pei Y, Zhu L, Xu Q. Three-dimension correction of Charcot ankle deformity with a titanium implant. Comput Assist Surg (Abingdon). Dec 2021;26(1):15-21. doi:10.1080/24699322.2021.1887356
2. Emara KM, Ahmed Diab R, Amr Hemida M. Tibio-calcaneal fusion by retrograde intramedullary nailing in charcot neuroarthropathy. Foot (Edinb). Mar 2018;34:6-10. doi:10.1016/j.foot.2017.11.003
3. Bajuri MY, Ong SL, Das S, Mohamed IN. Charcot Neuroarthropathy: Current Surgical Management and Update. A Systematic Review. Front Surg. 2022;9:820826. doi:10.3389/fsurg.2022.820826
4. van der Ven A, Chapman CB, Bowker JH. Charcot neuroarthropathy of the foot and ankle. J Am Acad Orthop Surg. Sep 2009;17(9):562-71. doi:10.5435/00124635-200909000-00003
5. Franceschi F, Franceschetti E, Torre G, et al. Tibiotalocalcaneal arthrodesis using an intramedullary nail: a systematic review. Knee Surg Sports Traumatol Arthrosc. Apr 2016;24(4):1316-25. doi:10.1007/s00167-015-3548-1
6. Pinzur MS, Kelikian A. Charcot ankle fusion with a retrograde locked intramedullary nail. Foot Ankle Int. Nov 1997;18(11):699-704. doi:10.1177/107110079701801104
7. Martin B, Chow J. The use of circular frame external fixation in the treatment of ankle/hindfoot Charcot Neuroarthropathy. J Clin Orthop Trauma. May 2021;16:269-276. doi:10.1016/j.jcot.2021.02.016
8. DeVries JG, Berlet GC, Hyer CF. A retrospective comparative analysis of Charcot ankle stabilization using an intramedullary rod with or without application of circular external fixator–utilization of the Retrograde Arthrodesis Intramedullary Nail database. J Foot Ankle Surg. Jul-Aug 2012;51(4):420-5. doi:10.1053/j.jfas.2012.03.005
9. Cinar M, Derincek A, Akpinar S. Tibiocalcaneal arthrodesis with posterior blade plate in diabetic neuroarthropthy. Foot Ankle Int. Jun 2010;31(6):511-6. doi:10.3113/fai.2010.0511 10. Zhang C, Shi Z, Mei G. Locking plate versus retrograde intramedullary nail fixation for tibiotalocalcaneal arthrodesis: A retrospective analysis. Indian J Orthop. Mar-Apr 2015;49(2):227-32. doi:10.4103/0019-5413.152492