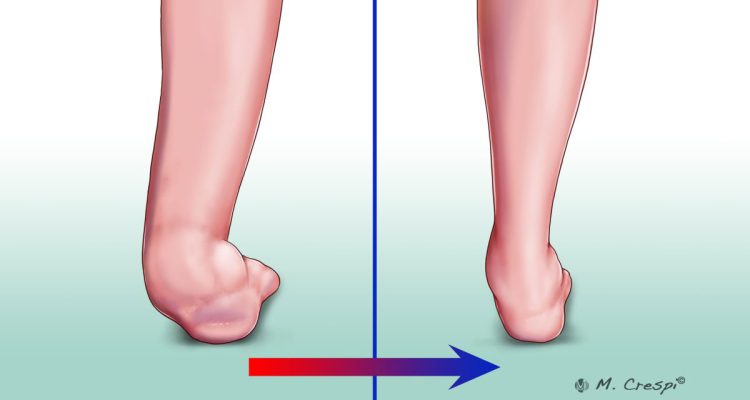
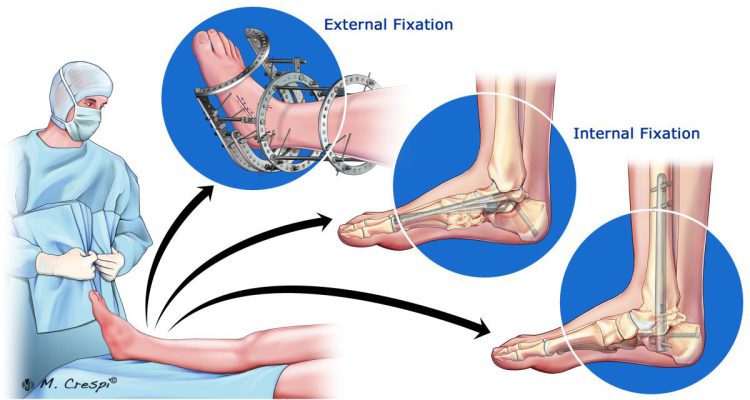
Charcot Foot and Ankle is a significant problem caused by peripheral neuropathy, with an estimated incidence of 0.3 to 7.5% in the diabetic population. This condition, which is also known as Charcot arthropathy, Charcot joint, or neuropathic arthropathy, affects the soft tissues, joints, and bones in the foot and ankle. If left untreated, it may lead to progressive foot deformity, ulceration, or osteomyelitis. In the most advanced stages, it may be necessary to resort to limb amputation.
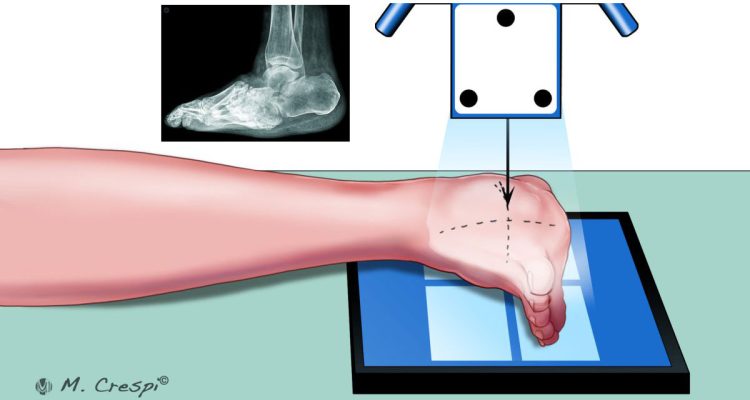
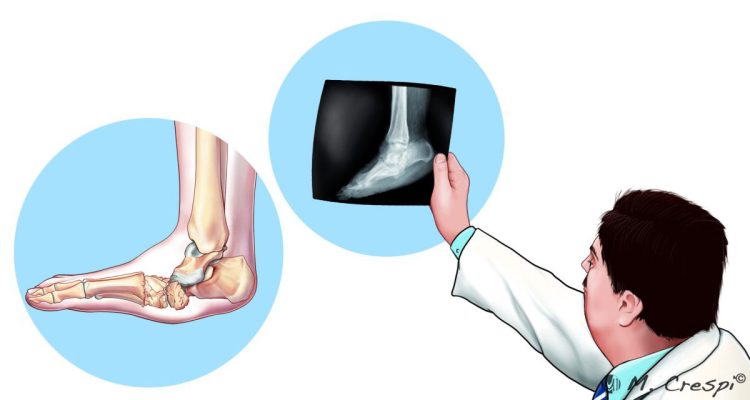
A rapid and accurate Charcot Foot diagnosis is important to prevent progressive and destructive deformity of the foot. The diagnosis includes clinical signs and specific Charcot Foot symptoms, but imaging tools also play a crucial role.
This article will focus on the use of Magnetic Resonance Imaging (MRI) to make an early diagnosis of Charcot Foot and Ankle.
Using MRI to Diagnose and Monitor Charcot Arthropathy
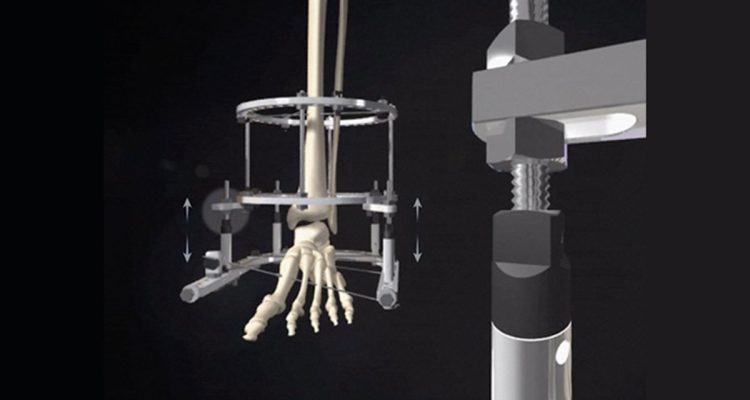
The use of MRI is becoming increasingly popular for the diagnosis of Charcot Foot and Ankle, especially in the early stage (Eichenholtz Stage 0), which is marked by inflammation. When applied to the musculoskeletal system, MRI provides excellent soft-tissue contrast resolution and multiplanar capabilities.
In the early, acute phase of Charcot Foot and Ankle, radiographic results may be normal, since the alterations caused by inflammation mainly affect the soft tissues; the bone damage will come later. MRI plays a vital role in the diagnosis to prevent this bone damage from occurring.
Performing an MRI is recommended when there is enough clinical suspicion for Charcot arthropathy. The results can demonstrate periarticular bone marrow edema, adjacent soft tissue edema, joint effusion, and microtrabecular or stress fractures.
The imaging protocol should include both T1 (defining anatomy) and short tau inversion recovery (STIR) sequences. The use of contrast (gadolinium 0.1 mmol/kg intravenously) is also recommended, mainly to improve diagnostic accuracy for the possible presence of osteomyelitis. The main findings with each sequence can be summarized as follows:
- T1: involved joints appear diffusely swollen, showing decreased signal intensity. There is also a decreased signal intensity in fat planes adjacent to ulcerated skin.
- T1 + gadolinium: inflammatory areas show enhancement, with central non-enhancing necrotic areas.
- STIR: in early infection there is increased signal intensity due to marrow edema, while later stages show a loss of demarcation of cortical outline and cortical destruction.
MRI can also be used to exclude the possibility of Charcot Foot and Ankle in a patient at risk, since a negative MRI indicates that acute Charcot joint is unlikely.
Involving the Patient in the Management of Charcot Arthropathy
Making a timely diagnosis in Charcot Foot and Ankle is challenging, especially in the early stage, when radiographic changes are not apparent. In these situations, the use of MRI can reveal subtle alterations in the soft tissues to the observant radiologist, allowing for quick implementation of preventative measures. MRI can also be used to assess whether the treatment is successful.
Nonetheless, the patient has a key role in the context of a Charcot Foot and Ankle. By being informed about the condition and keeping an eye to any alteration in his or her feet, the attentive patient can avoid the devastating complications of neuropathic arthropathy. The first step to start a diagnosis comes from the patient who has a good understanding of Charcot arthropathy and a good connection with the members of the multidisciplinary healthcare team.
To help your patients know more about Charcot Foot and Ankle, the available diagnostic tools, and their own role in the management of the disease, we suggest downloading the Patient Informative Cards “Stand On Your Feet: A Program of Empowerment for Your Diabetic Foot Management.”

References
- Mautone M, Naidoo P. J Med Imaging Radiat Oncol 2015 Aug;59(4):395-402.
- Marmolejo VS et al. Am Fam Physician. 2018 May 1;97(9):594-599.
- Rogers LC, Bevilacqua NJ. Clin Podiatr Med Surg 2008 Apr;25(2):263-74, vii.
- Schoots et al Semin Musculoskelet Radiol. 2010 Sep;14(3):365-76.