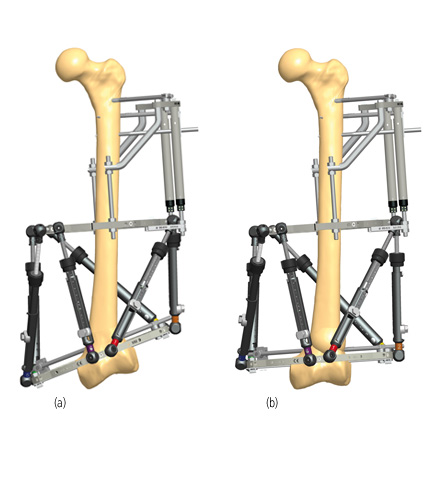
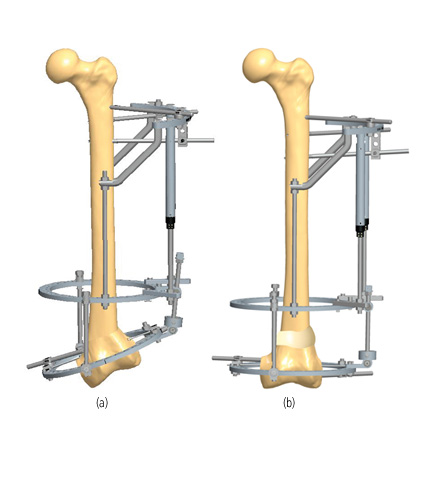
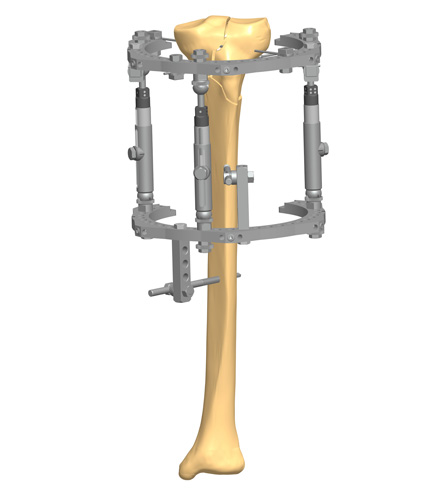
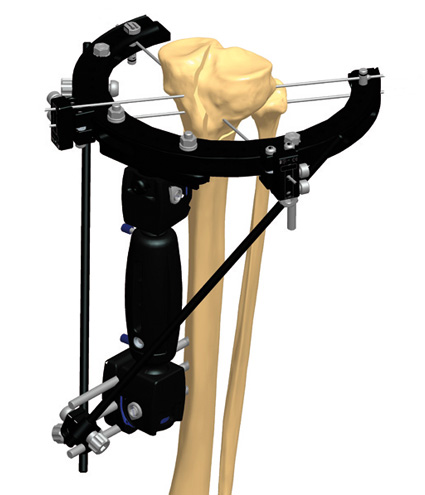
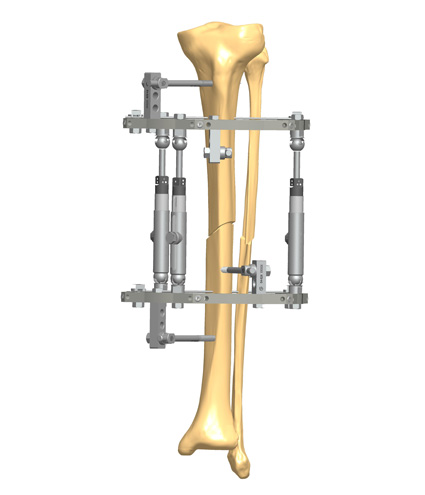
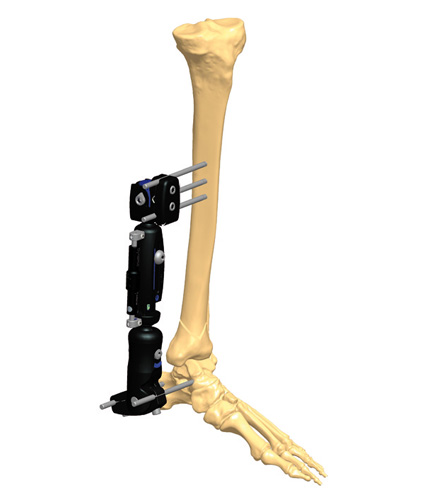
Stability does not mean rigidity. Medical philosophy has evolved from the aim to eliminate micromotion between the bony fragments to the idea of controlling it. Micromotion is necessary for external callus formation, and therefore for a functional bone healing. External fixation offers the opportunity to control both micromovement and load at the fracture site, which corresponds to the concept of dynamization.
The necessity of some element of motion for external callus formation is generally accepted.
Movement between fracture ends can be stimulatory or inhibitory depending on the motion’s magnitude.(1) Fractures of the femur treated in traction without a splint show some motion at the fracture site from the early days after injury, as well as fractures of tibia treated in cast with early weightbearing often heal with significant callus formation.(2) To the contrary, employing internal fixation with a plate and screws, or external fixation in combination with rigid internal fixation, inhibits or totally suppresses the external callus formation. Kenwright and Goodship have shown that controlled axial cyclic micromotion applied to tibial fractures decreased the time to full weightbearing, but it should be limited to less than 2mm to be effective.(3)
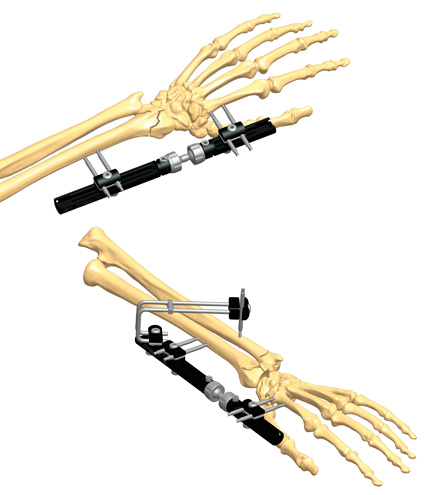
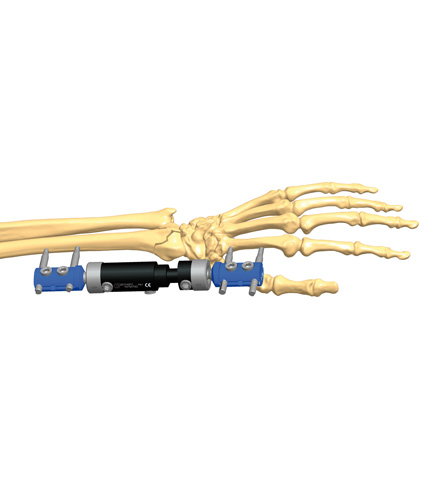
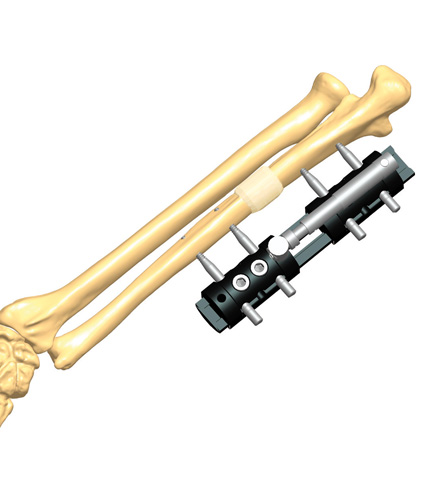
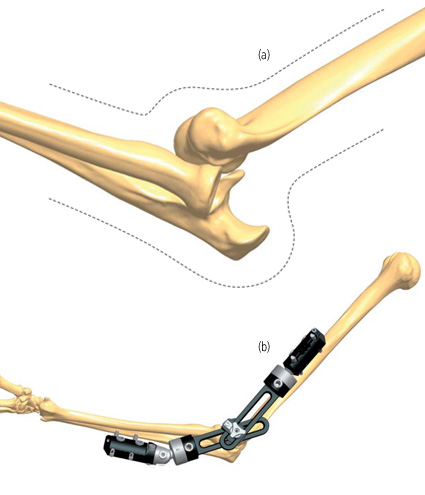
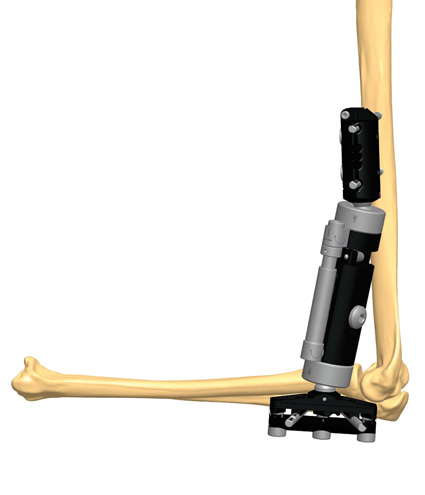
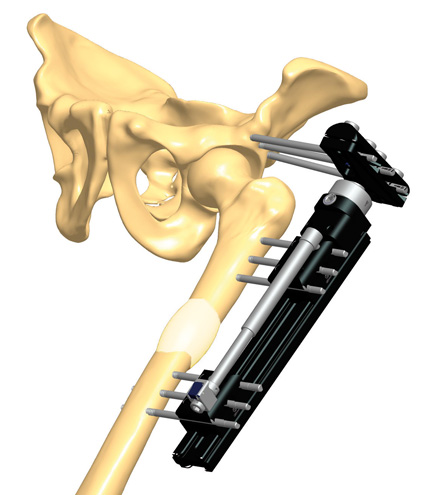
External fixation offers the opportunity to control both movement and load at the fracture site: this is the concept of dynamization, first recognized and defined by Giovanni De Bastiani, an Italian Professor of Physiology at the University of Padua, and later Professor of Orthopedics at the University of Verona.(4)
Dynamization means different methods (i.e. applied cyclic micromotion and progressive axial loading) of altering the fixation of fractures during the bone healing process to improve external callus formation.
In addition to that, numerous experimental and clinical studies have shown that both the amount of applied strain and the timing of application of the cyclic micromotion are critical.(5)
Considering the different phases of the fracture healing process, cyclic micromotion contributes to speeding up the callus formation, while progressive loading stimulates the callus maturation until full calcification of the callus, thus restoring the proper mechanical properties of the bone.
According to Prof. De Bastiani’s first indications, dynamization should start once the presence of early callus has been observed in the radiographs, in a stable fracture.
References
- Marsh DR, Gang Li 1999. The biology of fracture healing: optimizing outcome. British Medical Bulletin; 55(4):856-69.
- Sarmiento A, Gersten LM et al. 1989. Tibial shaft fractures treated with functional braces. Experience with 780 fractures. J Bone Joint Surg; 71B:602-9.
- Kenwright J, Goodship AE 1989. Controlled mechanical stimulation in the treatment of tibial fractures. Clin Orthop; 241:36-47.
- De Bastiani G, Aldegheri R et al. 1984. The treatment of fractures with a dynamic axial fixator. J Bone Joint Surg; 66B:535-45.
- Claes L 2018. Dynamisierung der Osteosynthese : Zeitpunkt und Methoden [Dynamyzation of fracture fixation : timing and methods]. Unfallchirurg; 121(1):3-9.