Charcot Neuroarthropathy, also called Charcot Foot and Ankle, is a progressive and inflammatory condition that weakens the soft tissues, bones, and joints of the foot and ankle. This complex and challenging type of neuropathic arthropathy is commonly linked to diabetes. If left untreated, it can lead to devastating consequences, such as deformity, ulceration, and infection. In the worst-case scenario, it may result in limb amputation.
Other names for Charcot Neuroarthropathy:
- Charcot joint
- Charcot arthropathy
- Neuropathic arthropathy
- Charcot arthropathy foot
- Charcot Foot and Ankle
In this article, we will explore the risk factors for developing Charcot Foot and Ankle, as well as the disease progression. We will also explain Charcot Foot and Ankle classification, based on the most recent data and research.
Who Can Develop Charcot Foot?
As mentioned before, diabetes is one of the major risk factors for developing Charcot Foot and Ankle, especially for patients who live with diabetes for a long time. This is due to the significant sensory peripheral neuroarthropathy that emerges in these patients. Among patients with diabetes, 0.3 to 7.5% may develop Charcot Foot and Ankle, which highlights the importance of continuous monitoring.
Despite the major link with diabetes, Charcot Foot and Ankle may also occur in patients with other diseases that are complicated by peripheral nerve damage, like leprosy. Men, especially those over 50 years old, are at increased risk of developing Charcot Neuroarthropathy. Other risk factors include poorly controlled blood sugar levels and lifestyle factors, such as long-term use of alcohol and smoking.
It is important to know that there is not a single cause for Charcot Foot and Ankle; instead, there are factors that predispose its development, and a number of triggering events.
Charcot Foot and Ankle Progression
When there is damage to peripheral nerves, the patient partially loses the ability to feel pain and temperature. Due to the decreased pain sensation, patients may be unaware of small traumas, continuing to walk on an injured foot.
The interplay between the several risk factors and the possibility of untreated traumas can result in an acute localized inflammation, where the foot is swollen, hot, and red, albeit without pain (due to the decreased pain sensation). The next phase involves bone loss (osteopenia) and fragmentation, accompanied by joint dislocation.
Bone fragmentation eventually resolves, even if swelling persists. By coalescing in an inappropriate form, there is a collapse of the midfoot arch, leading the foot to change shape (deformation). In the last phase, there is a consolidation of the deformity, causing the hallmark “rocker-bottom” foot.
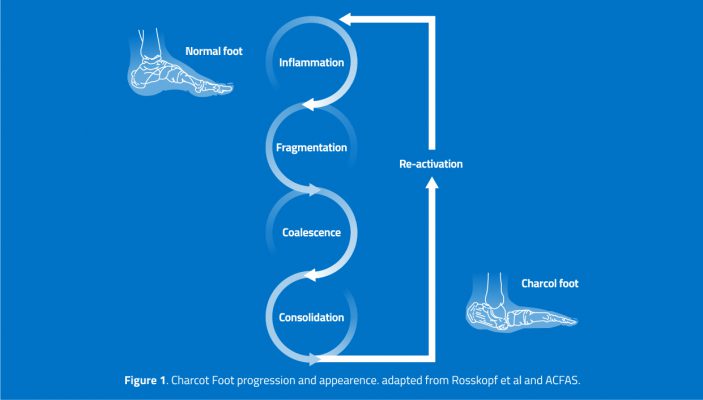
The natural course of Charcot Neuroarthropathy encompasses active and inactive disease phases, which relate to an inflamed or stable disease, respectively. After the consolidation phase, there is a 23% risk of “re-activation” of the inflammation phase, which leads to a progressively worse condition.
Classification of Charcot Foot and Ankle
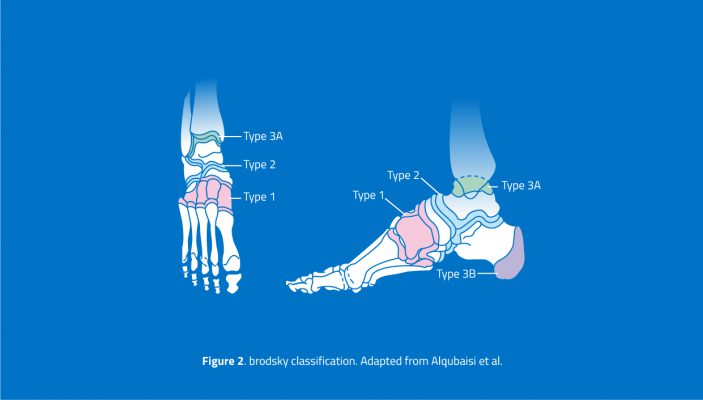
There are two main systems of classification of Charcot Neuroarthropathy: the modified Eichenholtz classification, which relies on clinical and radiographic findings, and the Brodsky classification, which focuses on the anatomical distribution of the affected regions.
The four stages of the modified Eichenholtz classification (0, 1, 2, and 3) correlate with the different phases of disease progression discussed earlier, and are frequently used in the clinical assessment of a suspected Charcot Foot and Ankle:
- Stage 0, where patients typically present with erythema and swelling, but no visible changes (yet) on radiographs. In these situations, the use of MRI can help the diagnosis.
- Stage 1 involves bone destruction, with radiographic evidence of debris formation, bone fragmentation, subluxation or dislocation.
- Stage 2 corresponds to the coalescence phase, with absorption of debris and sclerosis of the bony ends.
- Stage 3 is the consolidation phase, with remodeling of bone fragments, decreasing sclerosis, and partial reformation of the architecture of the foot and ankle.
According to the Brodsky classification, Charcot Neuroarthropathy usually begins in the tarsometatarsal (Lisfranc) and lesser tarsus region (Type 1), although it may also be seen in the transverse tarsal (Chopart), subtalar and peritalar (Type 2). Type 3a involves the ankle and tibiotalar joints, while Type 3b involves the posterior calcaneum, with a compromised longitudinal arch and Achilles’ insufficiency. Trepman later added Type 4 and Type 5, to describe the involvement of multiple sites and the forefoot (metatarsophalangeal), respectively.
Conclusion
Charcot Neuroarthropathy is a complex syndrome, often a complication of diabetes and peripheral neuropathy. Its destructive potential starts with inflammation, as a result of unnoticed foot trauma. The classic “rocker-bottom” deformity manifests in a late phase, but can be avoided with timely recognition and treatment.
To know more about the diagnosis and management of Charcot Foot and Ankle, read the article “The Stages of Charcot Foot and Ankle Disease and The Importance of a Quick Diagnosis.”

References
- Rosskopf AB et al. Insights Imaging. 2019 Aug 5;10(1):77.
- American College of Foot and Ankle Surgeons (ACFAS) 2017.
- Marmolejo VS et al. Am Fam Physician. 2018 May 1;97(9):594-599.
- Dardari D. J Clin Transl Endocrinol. 2020 Oct 28;22:100239.
- Korzon-Burakowska A, Dziemidok P. Ann Agric Environ Med. 2011;18(2):314-7.
- Capobianco CM et al. J Orthop Surg Res. 2010 Feb 11;5:7.
- Alqubaisi M et al. Int J Foot Ankle 2018, 2:021.
- Baravarian B, Van Gils CC. Clin Podiatr Med Surg. 2004 Apr;21(2):271-89.
- Shibata T et al. J Bone Joint Surg Am. 1990 Jun;72(5):749-56.