Dynamization (dynamic loading and controlled motion at the fracture site) is considered a controversial and evolving issue, besides the positive functional results observed both in experimental studies based on animal models, and in human clinical cases in the last 30 years. Currently one crucial matter is to understand the biomechanical, biological and physiological effects of dynamization on the bone healing process, in order to show its safety and effectiveness.
Looking at the extensive literature on the role of dynamization , one comes across some basic concepts. The first one is the concept of strain, which is strongly related to the callus formation process, as it is well known that mechanical environment and physical forces alter cells’ differentiation and metabolism: “strain is first and foremost appropriate way of understanding fracture healing and improving treatment”.(1) The theory holds that strain < 2% is well tolerated by lamellar bone; between 2 and 10% is better tolerated by woven bone. Too much strain means no callus induction. In practice, a sort of “middle way theory”, the so-called “Lagom theory” which comes from a Swedish word meaning balance: not too much, neither too little, just enough.(2)
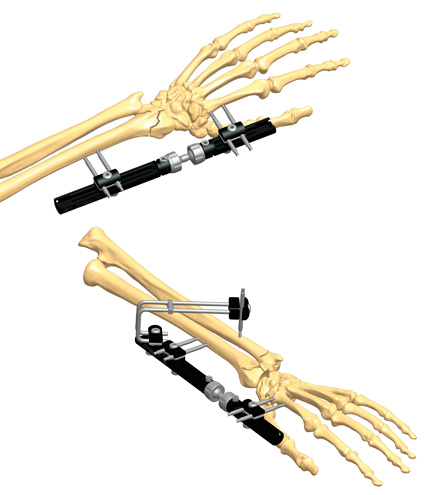
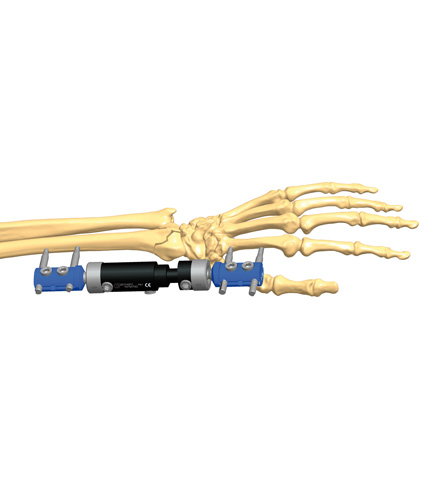
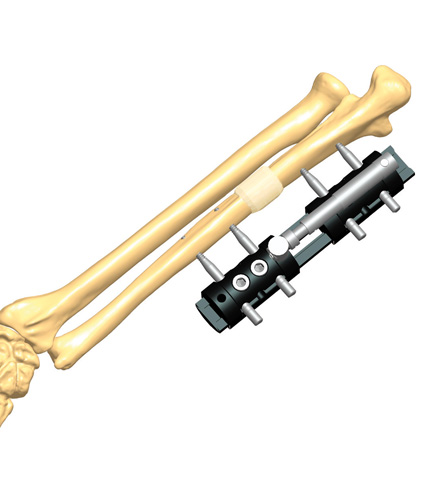
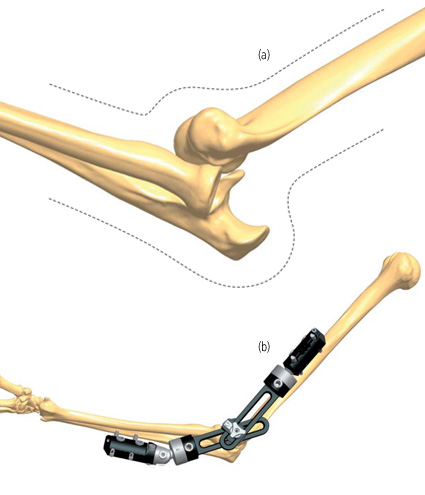
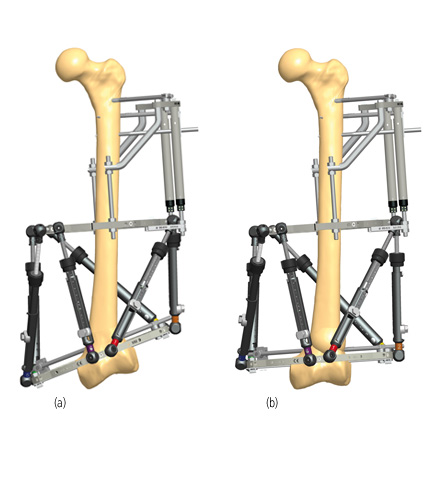
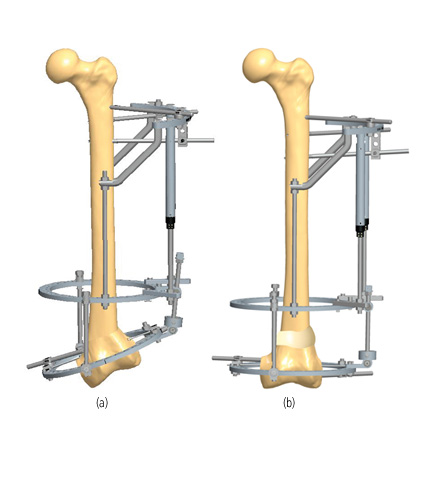
A further point is the need to define what one means with the term dynamization, as it affects the outcome: axial dynamization, or elastic dynamization, as each method is related to the chosen dynamization strategy. The conventional dynamization regime means compression followed by dynamization. The reverse dynamization regime means early motion to stimulate callus, followed by rigidity: some recent studies have shown that this regime gives superior results.(3)
Other studies have shown that late dynamization after 12 weeks, is still beneficial to promoting healing in femoral and tibial diaphyseal fractures using intramedullary interlocking nailing, while comminuted fractures show poor results with dynamization.(4) It also has been observed by some experts that dynamization works well in the presence of acute fractures, so it may be considered as first line treatment for delayed union and non-union.
Timing is another key factor in dynamization. Numerous experimental and clinical studies have shown that both the amount of applied strain and the timing of application of the motion are critical for the callus formation,(5) (6) and this is related to the patient’s age, gender and physical condition, as well as to the fracture type, that have to be individually assessed.(7)
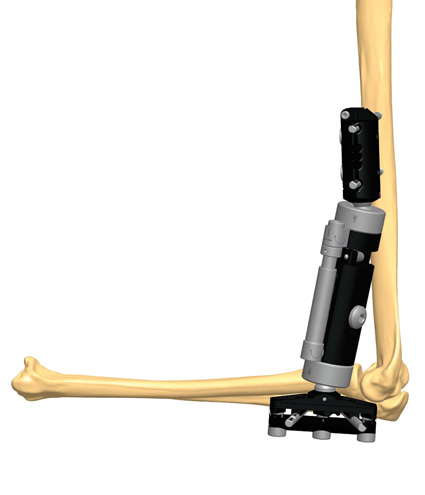
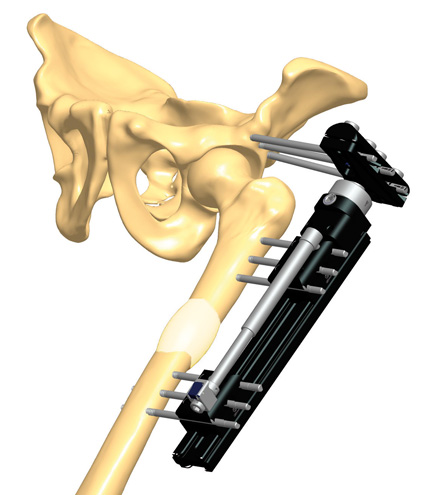
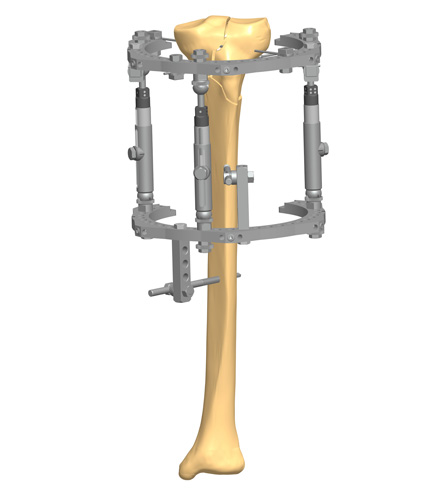
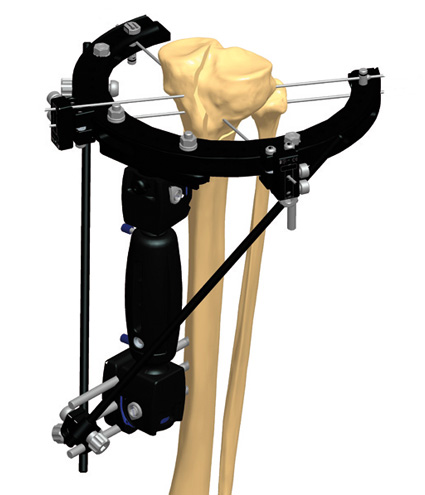
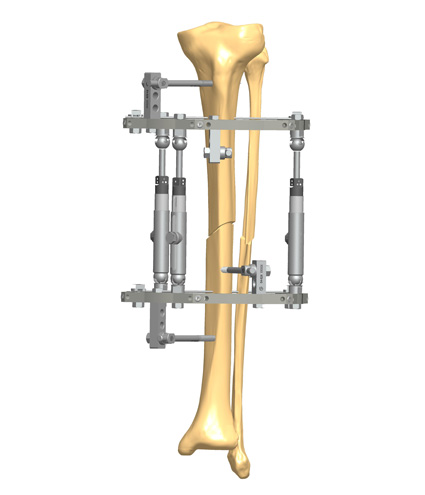
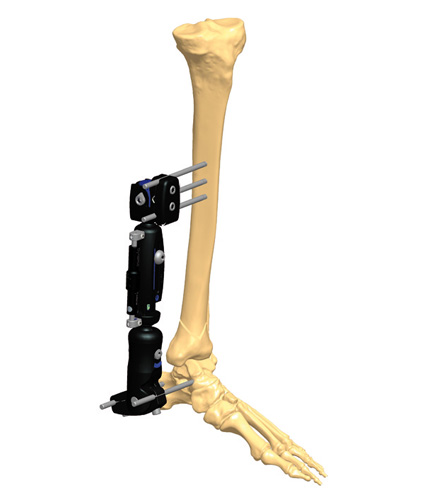
Encouraging results obtained using experimental animal models, especially large ones such as goats, seem to validate the safety of controlled dynamization and its effectiveness in the bone healing process.(6) (8) In the clinical practice with human patients, this becomes even more evident: applying dynamization when using a circular external fixator, during the whole period of treatment – with small degrees of controlled axial micromotion and loading (due to some innovative dynamization modules) – may promote blood flow at the fracture site, reduce discomfort, accelerate the fracture healing process, and require shorter rehabilitation after frame removal.(9) (10)
References
- Perren S, Fernàndez A et al. 2015. Understanding Fracture Healing Biomechanics Based on the “Strain” Concept and its Clinical Applications. Acta Chir Orthop Traum Cech; 82(4)253-60.
- Ferreira N, Tanwar YS et al. The effect of Fixation Dynamization on Fracture Healing: A Systematic Review. J Limb Length Recon; 6(1):7-12.
- Howard et al 2013. Fracture healing? A pilot study in tibial fractures. J Traum Treat; 2(4):176.
- Perumal R, Shankar V et al. 2018. Is nail dynamization beneficial after twelve weeks? An analysis of 37 cases. J Clin Orthop Traum; 9(4):322-6.