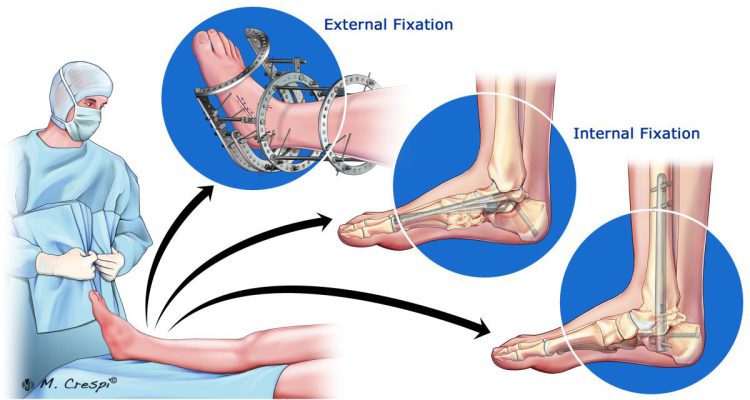
When dealing with Charcot Foot Disease, a swift diagnosis is crucial to improve patient outcomes and avoid complications such as foot deformity, ulceration, and in a worst-case scenario, limb amputation. However, not all physicians are able to recognize the initial signs of a Charcot Foot and Ankle in their diabetic patients.
As a general rule, a diagnosis of acute Charcot Foot and Ankle should be considered in any patient who is 40 years or older with obesity and peripheral neuropathy, who presents a unilateral swollen limb and minimal or no pain. The main difficulty in establishing a diagnosis is that the acute signs and symptoms can be similar to other conditions, often leading to a misdiagnosis and delayed treatment.
In this article, we will explore the different stages of this pathology, highlighting the most important symptoms for each stage and analyzing what diagnostic tools are available.
The Different Stages of Charcot Foot and Ankle
The natural course of Charcot Foot and Ankle is characterized by four stages, and the patient can cycle through them in a pattern resembling active and inactive phases, resulting in high morbidity and accentuated foot deformity.
An early stage Charcot Foot and Ankle can be defined by the presence of inflammation, triggered by an injury or trauma that went unnoticed. As the patient continues to walk on an injured foot, the inflammation becomes generalized, resulting in a hot, red, and swollen foot, albeit many times without pain due to the underlying polyneuropathy.
After the initial inflammation stage and if not properly managed, there is a progression toward other Charcot Foot stages, as follows:
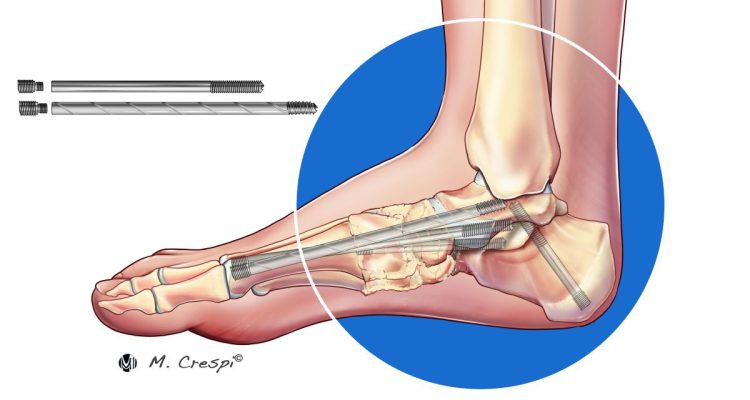
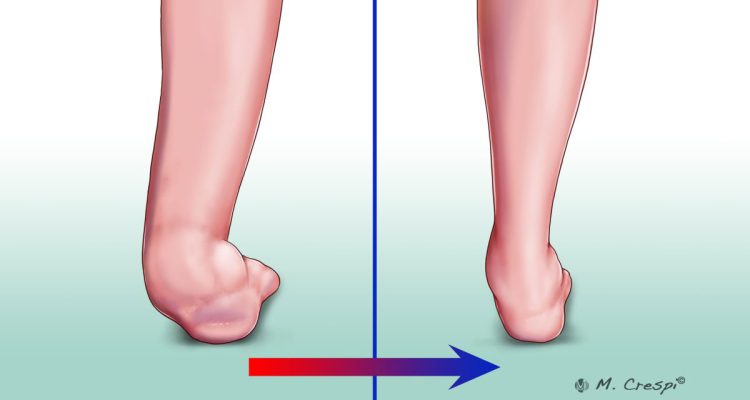
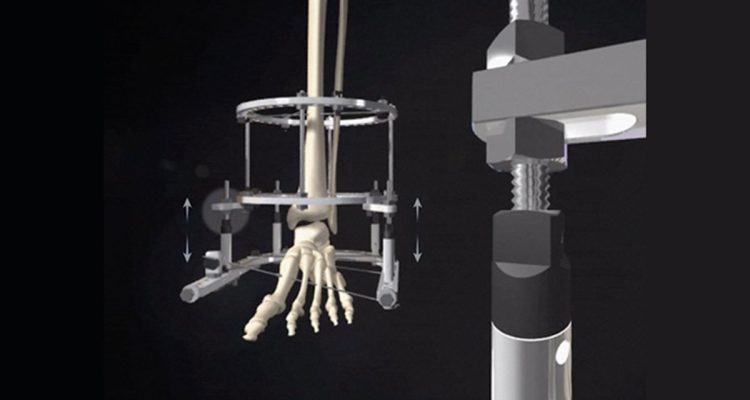
- Fragmentation: the fragilized bone fractures, leading to joint dislocation and collapse of the foot arch. In this stage, there is radiographic evidence of debris formation, bone fragmentation, and subluxation.
- Coalescence: erythema often resolves in this stage, but swelling may persist. Radiographs show debris absorption, fusion of larger bone fragments, and sclerosis of bony ends.
- Consolidation: this is the reconstruction stage, with remodeling of bone fragments. The deformity caused by bone fracture consolidates, and there is radiographic evidence of decreasing sclerosis, joint arthrosis, and partial reformation of the architecture of the foot and ankle. The physical exam shows absence of swelling and erythema, and the joint is more stable (in the context of a fixed deformity).
During the coalescence and consolidation stages, the inflammation gradually subsides, leading to a less active phase of the disease. While some patients only cycle once through the four stages, there is a 23% risk of re-activation of the inflammatory (active) phase, with a mean interval of 27 months. In these cases, the patient re-enters the cycle with inflammation, resulting in further foot deformity if not appropriately treated.
In a patient with diabetes, the potential for developing Charcot Foot Disease is intensified by the complex relationships between blood sugar levels, vascular disease, and peripheral neuropathy.
Making an accurate Charcot Foot diagnosis in this early stage might be difficult, since the acute symptoms can be similar to other conditions, such as cellulitis, gout, or deep vein thrombosis. In these circumstances, the use of imaging tools can help confirm Charcot Foot Disease, as well as identify diabetic foot early stages.
How to Make a Charcot Foot Diagnosis
There are four domains involved in the diagnosis of Charcot Foot and Ankle:
- Clinical assessment, including a physical exam and patient history;
- Peripheral neuropathy exam;
- Initial imaging and laboratory values;
- Charcot Foot and Ankle stage confirmation.
In the physical exam, the clinician should look for signs of inflammation, such as edema, erythema, or elevated temperature. Ulceration, deformity, and pain may or may not be present. The patient history should include recalling any traumatic event, diabetes, alcoholism, etc., that could indicate potential peripheral neuropathy.
The peripheral neuropathy exam will assess the cutaneous sensitivity with Semmes-Weinstein Monofilament. The presence of decreased proprioception, delayed or absent vibratory sensation, absence of Achilles Tendon reflex, decreased muscle strength, and skin changes such as xerosis are indicative of peripheral neuropathy.
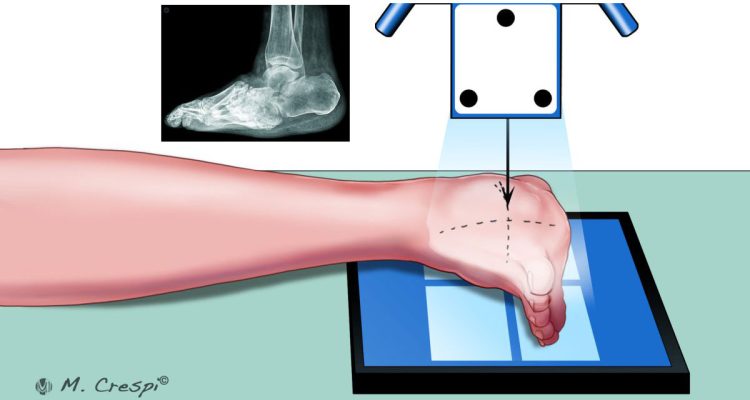
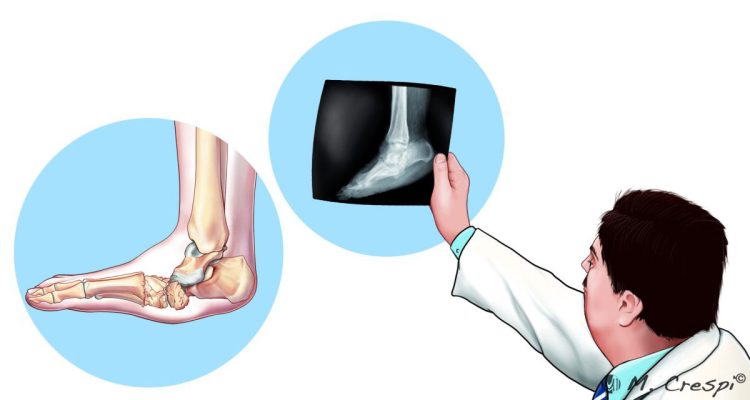
Radiographic imaging is commonly used to look for evidence of bone involvement, but in the stage 0 (early stage) there are no radiographic alterations yet. The use of Magnetic Resonance Imaging (MRI) to confirm Charcot Foot Diagnosis is therefore recommended, showing periarticular bone marrow edema of multiple bones even in this stage. Additional exams that may be performed include Radionuclide Imaging and Computerized Tomography (CT) to detect whether there are bone infections or additional signs that are not detectable through MRI.
The laboratory investigation should include hemoglobin A1c, fasting and/or random glucose, complete blood count, erythrocyte sedimentation rate, and C-reactive protein (CRP).
The early stage Charcot Foot is diagnosed with the help of MRI, while the more advanced stages are confirmed clinically and radiographically.
Conclusions
Making a timely diagnosis in a patient with Charcot Foot and Ankle can avoid serious complications, including limb amputation. However, early stage Charcot Foot signs and symptoms may be similar to other conditions.
Radiograph imaging is the standard technique to diagnose, stage, and monitor the disease, but do not show changes in the inflammatory stage. In this case, MRI is very useful to establish an early diagnosis and to monitor active versus inactive phases of the disease. In some cases, it is necessary to resort to CT and nuclear medicine (Radionuclide) imaging.
The patients also play a key role in the management of their disease, and it is vital to make them aware of their importance. Patients should be attentive to feet care, and promptly communicate any alteration to their healthcare team. To help your patients understand Charcot Foot and Ankle and their role, we suggest downloading the patient informative cards titled “Stand On Your Feet: A Program of Empowerment for Your Diabetic Foot Management.”

References
- Rosenbaum AJ, DiPreta JA. Clin Orthop Relat Res. 2015 Mar; 473(3): 1168–1171.
- Alqubaisi M et al. Int J Foot Ankle 2018, 2:021.
- Baravarian B, Van Gils CC. Clin Podiatr Med Surg. 2004 Apr;21(2):271-89.
- Rosskopf AB et al. Insights Imaging. 2019 Aug 5;10(1):77.
- Marmolejo VS et al. Am Fam Physician. 2018 May 1;97(9):594-599
- Vopat ML et al. Kans J Med. 2018 Nov 29;11(4):114-119