Charcot Foot and Ankle, also known as Charcot arthropathy, neuropathic arthropathy or Charcot joint, is a progressive condition that affects the bones, joints and soft tissue of the foot and ankle. It is caused by peripheral neuropathy. Today, diabetes is the most common cause for developing Charcot Foot and Ankle.
If left untreated, Charcot Foot and Ankle may lead to serious complications, including severe deformation, ulceration, and infection. In a worst-case scenario, amputation may be necessary. Making an accurate and timely Charcot Foot diagnosis is essential to avoid these complications and improve patient outcomes, especially those already living with the burden of diabetes.
The diagnosis of Charcot Foot and Ankle involves a clinical assessment, an exam to evaluate the presence of peripheral neuropathy, initial imaging and lab tests, as well as the disease stage confirmation. The imaging tools, namely radiographs, are fundamental in the diagnostic process in all stages of the disease. In this article, we will explore the use of radiography in the diagnosis of Charcot arthropathy.
Radiographic Findings in Neuropathic Arthropathy
One of the key diagnostic tools in Charcot Foot and Ankle is weightbearing radiography, and the radiologist plays an important role in the diagnosis and monitoring of the disease, particularly in the context of a multidisciplinary team.
Although radiographic findings are scarce or non-existent in the inflammatory stage (called stage 0 in the Eichenholtz Classification), a lack of evidence in this stage should not be used to rule out a possible Charcot Foot and Ankle problem. The radiographs collected at this stage serve as a baseline, and it may be possible to distinguish signs such as increased soft tissue volume or subtle subluxations. At this stage, if there are clinical signs and suspicion based on the patient’s risk profile, Magnetic Resonance Imaging (MRI) can also be used to make a Charcot Foot diagnosis.
In stage 1 (fragmentation), the earliest finding in plain radiographs is focal bone demineralization. It is also possible to note debris formation at the articular margins, fragmentation of subchondral bone, capsular distension, subluxation, dislocation and periarticular fractures.
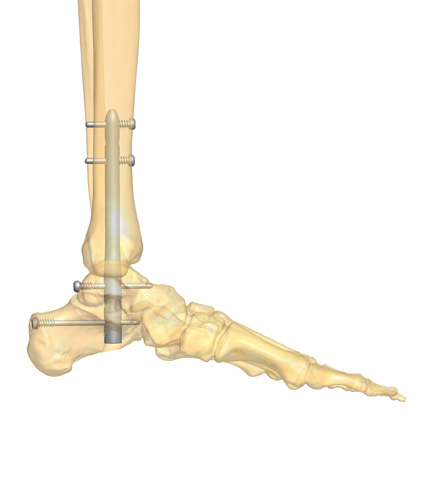
From a radiographic standpoint, stage 2 (coalescence) shows the absorption of fine debris and fusion of large fragments to adjacent bones and/or formation of new periosteal bone. In the last stage (stage 3, consolidation), radiographs show remodeled fragments, rounded bone ends, decreased sclerosis, and partial reformation of the architecture of the bone and ankle, with a fixed deformity.
The use of radiographs is indispensable in the advanced stages of Charcot Foot and Ankle, since it allows the correct identification of the disease stage, and also because it enables the monitoring of the disease activity and complications.
Communicating With the Patient
When dealing with Charcot Foot and Ankle, awareness is the key for ensuring a timely diagnosis. Clinicians should ask indispensable questions to their patients, such as relevant history of diabetes or peripheral neuropathy, look for signs and symptoms of an active Charcot Foot or other diabetic foot problems, and teach their patients to care for their feet and go for regular foot evaluations.
When assessing patients at their regular checkups, it is also important to know when to refer them to a specialist. This referral will have a different priority level, depending on factors such as sensitivity, presence or absence of ulcers, foot deformity, and others. A patient with satisfactory sensitivity, no ulcers, and no peripheral disease will be on the “very low” priority spectrum, needing a referral within the next three months for foot care and preventive foot health behavior education. On the other end of the priority spectrum (“very high”), a patient with open wounds, deep ulcers, pain at rest, an active Charcot Foot and Ankle deformity, and vascular compromise will need urgent/immediate referral to receive interdisciplinary care management, off-loading and/or surgery.
Charcot Foot symptoms can overlap with those seen in other conditions, such as a simple sprain or gout, especially in an early phase of the disease. In these circumstances, the attentive radiologist may assist in prompt intervention, since plain radiographs are the most commonly used imaging tool for diagnosis, staging and monitoring the evolution of Charcot arthropathy.
However, the patient with Charcot Foot and Ankle also has a key role in the disease management. Since the active, initial stage is driven by a state of inflammation, it is up to the patient to maintain an active vigilance regarding feet care and promptly communicate any alteration.
The complications of Charcot Foot and Ankle are devastating, and present an increasing socioeconomic challenge in today’s society. By involving patients in the management of their disease and creating a good rapport with all the members of the multidisciplinary team, there is a potential to improve outcomes, especially limb salvage.
If you would like to provide some reading material to your patients, we suggest downloading the Patient Informative Cards “Stand On Your Feet: A Program of Empowerment for Your Diabetic Foot Management”

References
- Mautone M, Naidoo P. J Med Imaging Radiat Oncol 2015 Aug;59(4):395-402.
- Rogers LC, Bevilacqua NJ. Clin Podiatr Med Surg 2008 Apr;25(2):263-74, vii.
- Moulik PK et al. Diabetes Care. 2003 Feb;26(2):491-4.
- Yablon CM et al. Curr Probl Diagn Radiol. Sep-Oct 2010;39(5):187-99.
- Marmolejo VS et al. Am Fam Physician. 2018 May 1;97(9):594-599.