The diagnosis of Charcot neuroarthropathy of the foot and ankle can be challenging due to a lack of information in the patient’s history, clinical assessment, imaging, and laboratory findings1. It is assumed that one in four cases of acute foot and ankle Charcot are undiagnosed or misdiagnosed1. However, correct diagnosis and effective treatment are crucial to avoid ulceration, worsening deformity, infection, or amputation1.
This article focuses on the recommendations from Charcot-specialized clinical experts on how to medically diagnose foot and ankle Charcot.
Always Be Suspicious
The best safeguard to avoid missing a presentation of foot or ankle Charcot is to always be suspicious2. The following clinical signs were summarized in a practical guideline about the surgical management of neuropathic Charcot foot2:
- Clinical signs of inflammation: patients with acute Charcot often present with a warm, swollen, and sometimes erythematosus and red foot. The diagnosis of foot and ankle Charcot should be suspected in every patient with diabetes and/or neuropathy who presents with these symptoms.
- Additional clinical signs are concomitant ulceration or crepitus during examination with patients often reporting a series of minor trauma.
- Many patients do not experience any pain in the foot.
We have asked some clinical experts to share their experience on Charcot diagnosis including their knowledge about the most common symptoms, the most misleading ones and about the evolution of the pathology.
The first recommendation from Lisa Grant-McDonald (DPM, Doctors Grant Foot & Ankle, Virginia Beach) was “Be suspicious, not only for patients with diabetes but for every neuropathic patient.”
Looking at the first steps of diagnosing Charcot foot, Stephanie Oexeman (DPM, Oexeman Foot & Ankle, Chicago) says: “I always start with the patient history and clinical signs such as erythema, edema, and increased temperature compared to the contralateral side. Typical red flags are increased sensation or pain in a typical neuropathic patient or repeated insignificant trauma.”
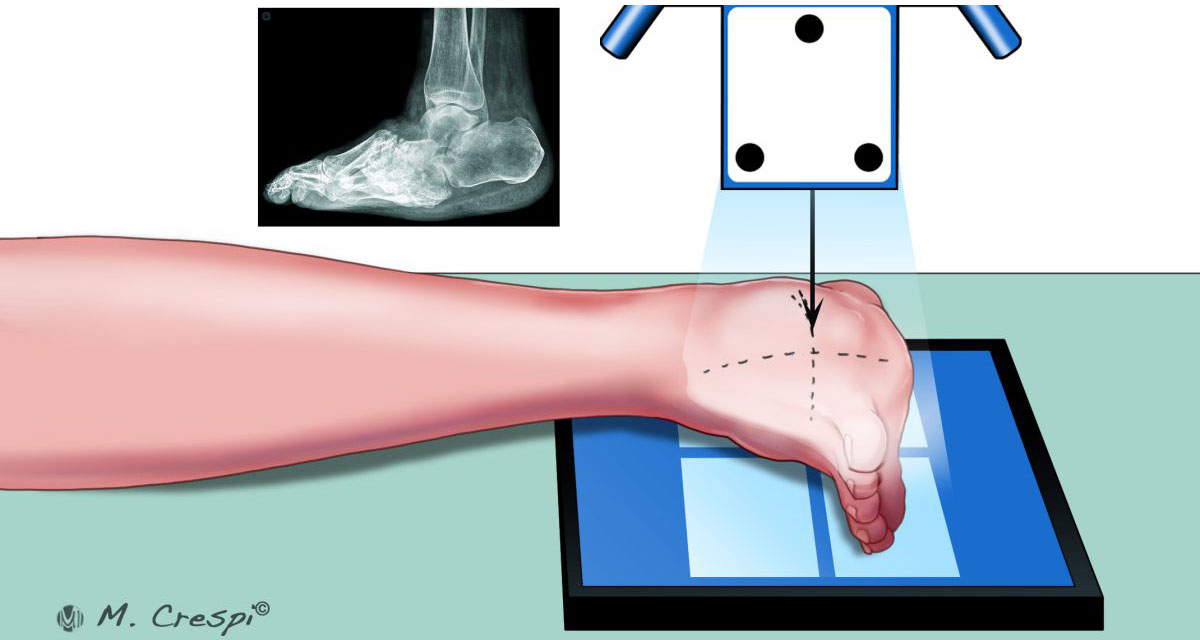
“Typical early signs of Charcot foot are heat and swelling, – adds Mohammad Sharif (DPM, Village Podiatry, Atlanta). – X-ray is the most relevant diagnostic tool as it shows early signs of diastasis at the joints.”
Besides the clinical assessment, the following imaging techniques are recommended2:
- Radiography: Plain and serial X-rays help identify demineralization, bone destruction, and periosteal reaction.
- Radionuclide (isotope) imaging: A high diagnostic value indicates if there is a penetrating ulcer underneath the deformity.
- Computerized Tomography (CT): Typical signs identified with CT are joint destruction, sequestra, cortical destruction, periosteal reaction, and intraosseous gas.
- Magnetic Resonance Imaging scans (MRI): A very high sensitivity for detecting abnormalities, especially in the soft tissues, but low specificity.
In addition to these standard diagnostic tests, Stephanie Oexeman (DPM, Oexeman Foot & Ankle, Chicago) uses another tool: “Thermography is an additional diagnostic tool to measure the temperature and assess differences between the limbs. The results can be saved with an app for better surveillance.”
Regular follow-ups are crucial, as confirmed by Mohammad Sharif (DPM, Village Podiatry, Atlanta): “I usually do follow-ups with additional X-rays every 2 to 4 weeks as long as the patient is immobilized.”
Daniel Scott (MD, MBA Medical University of South Carolina (MUSC) Orthopaedics, Charleston) also considers radiographic imaging for monitoring purposes: “My patients usually undergo X-rays every 2 to 4 weeks after the initial presentation to monitor transitioning from total contact casting to a custom bracing. I mainly use CT scans for preoperative planning and not for monitoring purposes.”

The Modified Eichenholtz Classification
Eichenholtz was the first to describe the different stages of Charcot foot in 1966. He reported a progression from the acute or fragmentation phase (stage I) to the subacute or coalescence phase (stage II) and the final consolidation and reconstructive phase (stage III). The modified Eichenholtz classification in Table 1 provides an overview of radiographic and clinical findings of each stage3.
Table 1: Modified Eichenholtz classification3
Stage |
Radiographic findings |
Clinical findings |
0 (prodromal) |
Normal radiographs | Swelling, erythema, warmth |
I (fragmentation) |
Osteopenia, fragmentation, joint subluxation, or dislocation |
Swelling, erythema, warmth, ligamentous laxity |
II (coalescence) |
Absorption of debris, sclerosis, fusion of larger fragments |
Decreased warmth, decreased swelling, decreased erythema |
III (reconstructive) |
Consolidation of deformity, joint arthrosis, fibrous ankyloses, rounding and smoothing of bone fragments |
Absence of warmth, absence of swelling, absence of erythema, stable joint ± fixed deformity |
More information about classification systems can be found in our article about definitions and medical classification.
Best Practice Tips
Marmolejo et al. summarized their key recommendations for clinical practice based on their expert consensus and scientific literature1:
- Acute Charcot neuroarthropathy should be suspected in every patient with the following characteristics and symptoms:
- > 40 years
- Obesity and neuroarthropathy
- Swollen unilateral limb with no or minimal pain.
- Acute Charcot neuroarthropathy should be suspected in patients with recurrent cellulitis without signs of infection.
- Besides clinical signs, weight-bearing X-rays of both feet are recommended to search for signs of impeding instability, such as subtle subluxations, joint destruction, or ligamentous avulsion.
The Most Relevant Differential Diagnoses
As described above, patients with acute foot or ankle Charcot usually present with an edematous, erythematous foot with increased temperature4. With these symptoms being non-specific, acute Charcot neuroarthropathy can be misdiagnosed for infectious, inflammatory or other diseases1. The following conditions should be considered1,4:
- Infections: cellulitis, erysipelas, osteomyelitis, septic arthritis
- Inflammation: acute inflammatory arthritis, gout, plantar fasciitis, pseudogout, rheumatoid arthritis
- Other diseases: fracture, sprain, venous insufficiency, deep venous thrombosis
In addition to these clinical signs, Daniel Scott (MD, MBA Medical University of South Carolina (MUSC) Orthopaedics, Charleston) explains the benefits of specific laboratory tests: “A tagged white blood cell scan is a helpful tool to differentiate Charcot foot from osteomyelitis (infection of bone).”
Unfortunately, no biomarkers or typical clinical signs differentiate acute Charcot of the foot from other conditions4. Therefore, continuous education and awareness of this devastating disease is so important4.
Further Reading
Charcot neuroarthropathy is a complex and challenging condition, and it is crucial to understand the underlying pathophysiological mechanisms for appropriate treatment5. Up-to-date resources on this challenging condition can be consulted here.

References
1. Marmolejo VS, Arnold JF, Ponticello M, Anderson CA. Charcot Foot: Clinical Clues, Diagnostic Strategies, and Treatment Principles. Am Fam Physician. May 1 2018;97(9):594-599.
2. Salvaterra P. The Surgical Management of Neuropathic (Charcot) Foot – A Practical Guideline. 2017;
3. Rosenbaum AJ, DiPreta JA. Classifications in brief: Eichenholtz classification of Charcot arthropathy. Clin Orthop Relat Res. Mar 2015;473(3):1168-71. doi:10.1007/s11999-014-4059-y
4. Schmidt BM. Clinical insights into Charcot foot. Best Pract Res Clin Rheumatol. Jun 2020;34(3):101563. doi:10.1016/j.berh.2020.101563
5. Trieb K. The Charcot foot. The Bone & Joint Journal. 2016;98-B(9):1155-1159. doi:10.1302/0301-620x.98b9.37038