Charcot foot is a progressive, devastating pathology defined by bone and joint changes that occur as a result of loss of sensation. Also called Charcot joint or neuropathic arthropathy, this condition is almost always associated with the vascular and neurological changes caused by poorly controlled diabetes1.
Although it was first diagnosed more than 130 years ago, diabetic Charcot foot remains a challenge for clinicians due to its rareness2. The estimated prevalence of Charcot joint is about 0.1% to 0.9% among patients with diabetes1,3,4. To put these numbers in context, for a prevalence of 0.56%, a general practitioner with 2,000 patients at his care and 100 patients with diabetes will have 0-1 patients with diabetic Charcot foot, and a new case every 13 years5.
Albeit rare, the consequences of neuropathic arthropathy can be catastrophic for patients: if unrecognized, disease progression may lead to ulcer formation, infection, and progression to active Charcot neuropathy, with joint instability and bone destruction6,7. In extreme cases, diabetic Charcot foot can result in limb amputation8,9.
Timely diagnosis is therefore essential, requiring an attentive clinician who is able to distinguish a Charcot joint from other pathologies such as erysipelas, cellulitis, acute gout, or peripheral vascular disease9. According to Mohammad Sharif, DPM, the combination of clinical signs and X-rays is the most common diagnostic approach to detect early Charcot. We dedicate other articles in this series to the medical diagnosis of Charcot arthropathy. In this text, we focus on the Charcot foot classification and definition.

What is Charcot Foot?
In January 2011, an international task force of experts was convened by the American Diabetes Association and the American Podiatric Medical Association to summarize available evidence on the pathophysiology, natural history, presentations, and treatment recommendations for this condition10.
The specialists defined the pathology as “a condition affecting the bones, joints, and soft tissues of the foot and ankle, characterized by inflammation in the earliest phase.” Following the acute inflammatory phase, the interaction of metabolic, neuropathic, and traumatic factors “may lead to varying degrees and patterns of bone destruction, subluxation, dislocation, and deformity”10.
The authors also describe the hallmark deformity known as “rocker-bottom” foot, where there is a midfoot collapse in advanced stages of Charcot neuropathic arthropathy (Figure 1).

Medical Classification of Diabetic Foot
The natural progression of diabetic Charcot foot typically follows three stages, as described by Eichenholtz in 1966:
- Stage I: acute or fragmentation phase
- Stage II: subacute or coalescence phase
- Stage III: consolidation and reconstructive phase
The first stage presents with evidence of osteopenia on radiographs, presence of periarticular debris or fragments, and joint subluxation or dislocation11. On physical examination, the affected joint will display swelling, erythema, and/or ligamentous laxity11. If the patient is in the second stage, their radiographs will show absorption of debris, early sclerosis, and bony consolidation of the larger fragments present in stage I, while clinical observation will reveal an apparent improvement of the condition, with decreased joint warmth and swelling11. In the last stage described by Eichenholtz, there is progression of the joint to a more stable structure, which presents as a fixed deformity on clinical examination, without any signs or symptoms of inflammation11.
Table 1 provides an overview of the Eichenholtz Charcot stages, with the addition of a stage 012 to reflect the observed clinical signs that precede radiographic changes.
Table 1: Modified Eichenholtz classification11
Stage |
Radiographic findings |
Clinical findings |
0 (prodromal) |
Normal radiographs | Swelling, erythema, warmth |
I (fragmentation) |
Osteopenia, fragmentation, joint subluxation, or dislocation | Swelling, erythema, warmth, ligamentous laxity |
II (coalescence) |
Absorption of debris, sclerosis, fusion of larger fragments | Decreased warmth, decreased swelling, decreased erythema |
III (reconstructive) |
Consolidation of deformity, joint arthrosis, fibrous ankyloses, rounding and smoothing of bone fragments | Absence of warmth, absence of swelling, absence of erythema, stable joint ± fixed deformity |
Other classification systems focus on the anatomical aspects of neuropathic arthropathy, such as those proposed by Sanders and Frykberg13 and by Brodsky and Rouse14. In these classifications, the authors propose patterns of joint involvement in the joint and ankle, which may occur individually or in conjunction with other areas. The Sanders and Frykberg classification describe type I to be the involvement of the metatarsophalangeal joints, type II occurs when the Lisfranc joint is affected, in type III the Chopart joint, and in type IV and V the subtalar joint and the calcaneus are involved, respectively13. The Brodsky and Rouse classification is now more widely used, and has somewhat different anatomical attributions.

Table 2: Brodsky anatomic classification of Charcot arthropathy foot
Type |
Location |
Involved joints |
1 |
Midfoot | Naviculocuneiform, tarsometatarsal |
2 |
Hindfoot | Subtalar, calcaneocuboid, talonavicular |
3A |
Ankle | Tibiotalar |
3B |
Calcaneus | Tuberosity fragmentation |
It can be difficult to distinguish between the different clinical stages of Charcot joint, and in this context, classification systems are important tools to promote communication among physicians16. Despite their age, all three classification systems described above have demonstrated good to excellent inter- and intrareader reliability16.
Further Reading
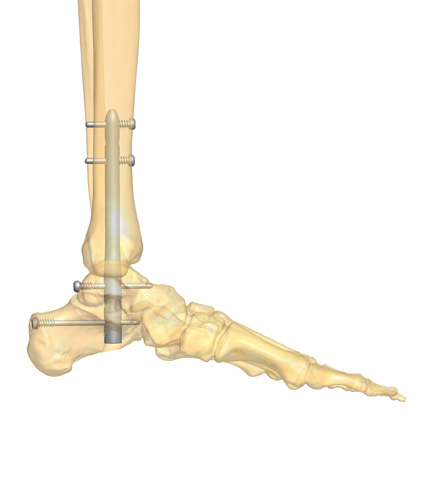
Charcot joint remains a serious complication of diabetes, with a complex presentation and guarded prognosis. It is fundamental to understand the underlying pathophysiological mechanisms in order to treat the condition appropriately9. Up to date resources on this challenging condition can be consulted here. To explore the surgical treatment of Charcot arthropathy foot, read our article on surgical approaches.

References
- Dardari D. An overview of Charcot’s neuroarthropathy. J Clin Transl Endocrinol. Dec 2020;22:100239. doi:10.1016/j.jcte.2020.100239
- Schmidt BM. Clinical insights into Charcot foot. Best Pract Res Clin Rheumatol. Jun 2020;34(3):101563. doi:10.1016/j.berh.2020.101563
- Fabrin J, Larsen K, Holstein PE. Long-term follow-up in diabetic Charcot feet with spontaneous onset. Diabetes Care. 2000;23(6):796-800. doi:10.2337/diacare.23.6.796
- Stuck RM, Sohn MW, Budiman-Mak E, Lee TA, Weiss KB. Charcot arthropathy risk elevation in the obese diabetic population. Am J Med. Nov 2008;121(11):1008-14. doi:10.1016/j.amjmed.2008.06.038
- Svendsen OL, Rabe OC, Winther-Jensen M, Allin KH. How Common Is the Rare Charcot Foot in Patients With Diabetes? Diabetes Care. 2021;44(4):e62-e63. doi:10.2337/dc20-2590
- Frykberg RG, Belczyk R. Epidemiology of the Charcot Foot. Clinics in Podiatric Medicine and Surgery. 2008/01/01/ 2008;25(1):17-28. doi:https://doi.org/10.1016/j.cpm.2007.10.001
- Wukich DK, Sung W, Wipf SAM, Armstrong DG. The consequences of complacency: managing the effects of unrecognized Charcot feet. Diabetic Medicine. 2011;28(2):195-198. doi:https://doi.org/10.1111/j.1464-5491.2010.03141.x
- Marmolejo VS, Arnold JF, Ponticello M, Anderson CA. Charcot Foot: Clinical Clues, Diagnostic Strategies, and Treatment Principles. Am Fam Physician. May 1 2018;97(9):594-599.
- Trieb K. The Charcot foot. The Bone & Joint Journal. 2016;98-B(9):1155-1159. doi:10.1302/0301-620x.98b9.37038
- Rogers LC, Frykberg RG, Armstrong DG, et al. The Charcot Foot in Diabetes. Journal of the American Podiatric Medical Association. 01 Sep. 2011 2011;101(5):437-446. doi:10.7547/1010437
- Rosenbaum AJ, DiPreta JA. Classifications in brief: Eichenholtz classification of Charcot arthropathy. Clin Orthop Relat Res. Mar 2015;473(3):1168-71. doi:10.1007/s11999-014-4059-y
- Shibata T, Tada K, Hashizume C. The results of arthrodesis of the ankle for leprotic neuroarthropathy. JBJS. 1990;72(5)
- Sanders L. Diabetic neuropathic osteoarthropathy: the Charcot foot. The high risk foot in diabettes mellitus. 1991;
- Brodsky JW, Rouse AM. Exostectomy for symptomatic bony prominences in diabetic charcot feet. Clin Orthop Relat Res. Nov 1993;(296):21-6.
- Mohamad A, Carlo R. Midfoot Charcot Neuroarthropathy. Int J Foot Ankle. 2018/12/31/ 2018;2(2)doi:10.23937/ijfa-2017/1710021
- Wukich DK, Raspovic K, Liu GT, et al. Are the Sanders-Frykberg and Brodsky-Trepman Classifications Reliable in Diabetic Charcot Neuroarthropathy? The Journal of Foot and Ankle Surgery. 2021;60(3):432-435. doi:10.1053/j.jfas.2020.03.003