Charcot Foot and Ankle is a complex, challenging and sometimes devastating inflammatory foot disease which causes loss of sensation, weakening of the bones and collapse of the weight bearing joints. Most often due to diabetes and underlying neuropathic arthropathy, it needs a multidisciplinary team approach in order to treat it properly and prevent amputation.
Charcot Foot and Ankle neuro-osteoarthropathy is a complex, multifactorial and often frustrating pathology, where the benefit of experience is somewhat of a double-edged sword that frequently leaves more questions than answers. In spite of this premise, basic principles and a golden standard approach, together with simple techniques and clear indications, are needed to help treat Charcot foot and ankle correctly, managing midfoot, hindfoot and ankle joints deformities, and preventing foot amputation.(1)
Today there is consensus on the following points:
1) Charcot Foot and Ankle management requires more surgery than it was thought before;
2) There is a pre-diabetes condition that often is under-diagnosed;
3) Foot and ankle ulcerations which occur frequently can be challenging when addressed surgically, after conservative care has failed;
4) Soft tissue coverage has a strong impact on Charcot reconstruction;
5) Concurrent immunopathy, angiopathy and peripheral neuropathy, accompanied by morbid obesity, may complicate the treatment approach and lead to foot amputation;
6) More than 50% of the amputations due to Charcot foot and ankle could be avoided;
7) A multidisciplinary team approach is mandatory. This team approach to the Charcot foot and ankle treatment – starting from the diagnosis – works both in preventing amputation and in reducing healthcare costs.(2)
Because of nerve damage due to diabetes, patients go on walking until the foot is compromised because they do not feel any pain. Ligaments do not function in the proper way, and biomechanical problems are often observed. Primary surgical treatment can be advantageous for the patient’s well-being: offloading with external fixation to prevent the risk of not having revascularization.
Osteomyelitis, frequently present in diabetic patients with Charcot as a result of foot ulcers, may require urgent surgery, but this is septic surgery and not yet Charcot reconstruction. Bone infections must be previously treated with antibiotics: staged salvage with prolonged targeted antibiotics until infection is eradicated.(3)
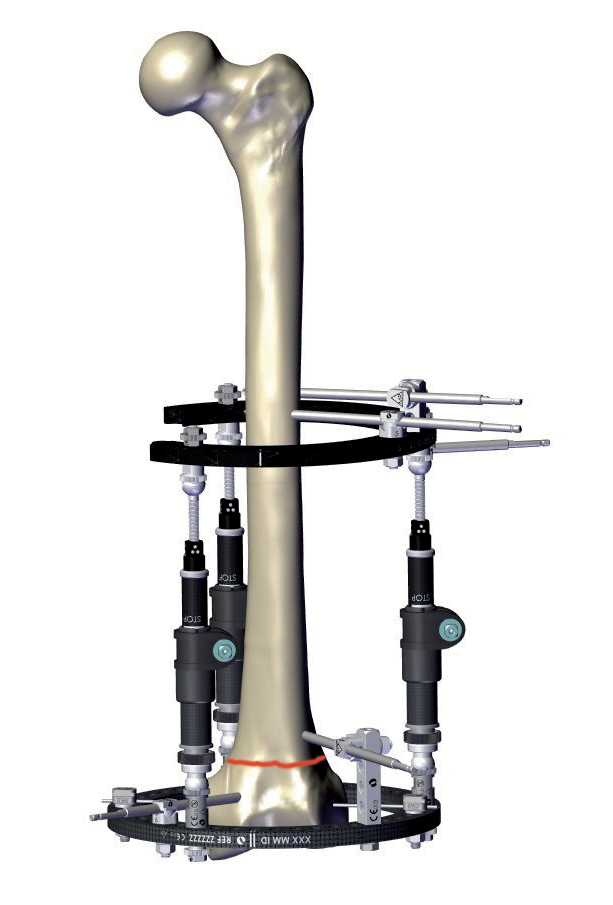
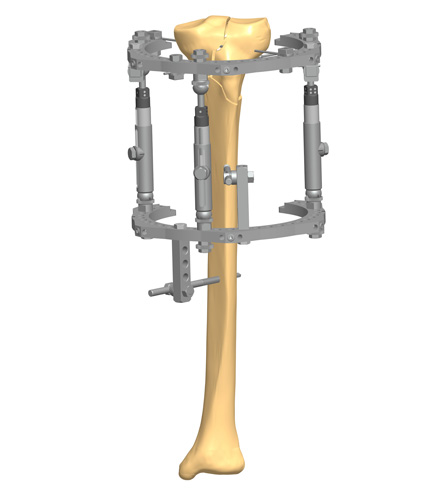
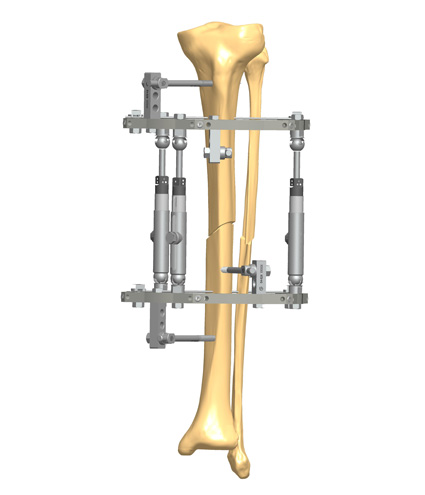
Reconstruction is indicated with an increased level of instability as well as multiplanar deformities, chronic wounds, chronic pain, and osteomyelitis. After bone debridement, the first stage of reconstructing a Charcot Foot and Ankle is to obtain correction – e.g. with acute or gradual soft tissues correction and osseous realignment, and the second stage is to maintain correction – e.g. with arthrodesis, especially when affecting the hindfoot, with the use of an external monolateral and/or circular frame.(4)
For Charcot midfoot reconstruction, more positive outcomes can be reached with a combination of internal and external fixation. Beaming or plating, and the use of an external fixator, is the suggested treatment. Sometimes a surgeon needs to stabilize the hindfoot in order to fix the midfoot: when isolated fusion doesn’t work, one has to fuse more segments – e.g. midfoot and hindfoot together. Plating may present the disadvantage of bad soft tissue condition, with a high risk of infections and revisions, as well as beaming.(5) (6)
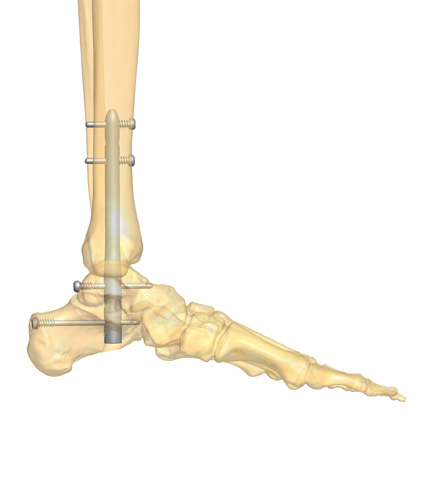
With ankle and subtalar dislocation, a suggested treatment is tibio-talo-calcaneal fusion by intramedullary nailing to hold the foot straight and stabilize the ankle joint. It can be done through small incisions, with lower soft tissue complications.(5)
Internal fixation is more suitable if the patient has no infected wounds, still good bone quality, intact soft tissue envelope.
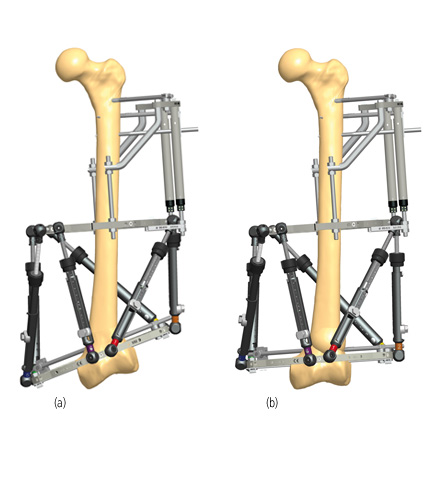
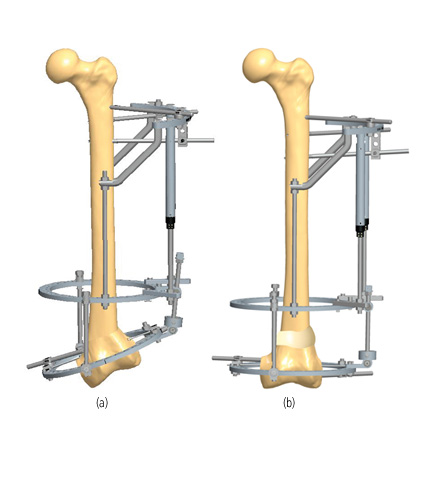
External fixation is recommended nearly always when deformity is present, and in the case of open wounds with active infection. Some advantages of this technique are that all the extraneous metal can be removed after 6-8 weeks; it is safer with open wounds; it works well in the acute Charcot foot and ankle management with dense peripheral neuropathy, and it provides stabilisation with ankle fractures and dislocations.(7) (8) It may be used in combination with internal fixation, when there is the need for supplemental fixation.
References
- Edmonds ME, Foster AVM, Sanders LJ 2008. A practical Manual of Diabetic Foot care, Blackwell Publishing, USA.
- Wukich DK, Amstrong DG et al. 2013. Inpatient Management of Diabetic Foot Disorders: a Clinical Guide. Diabetis Care, Sept; 36(9)2862-71.
- Koller A, Springfeld R et al. 2011. German-Austrian consensus on operative treatment of Charcot neuroarthropathy: a Perspective by the Charcot task force of the German Association for Foot Surgery, Diabet Foot Ankle; 2:10207.
- Baravarian B, Van Gills CC 2004. Arthrodesis of the Charcot foot and ankle. Clin Podiatr Med Surg; 21(2):271-89.
- Lee L, Blume PA et al. 2003. Charcot joint disease in diabetes mellitus. Ann Vasc Surg; 17(5):571-80.
- Ferreira RC, Gonçalez DH et al. 2012. Midfoot Charcot Arthropathy in diabetic Patients: Complication of an epidemic disease in Rev Bras Ortop. Sep-Oct; 47(5):616-25.
- Illgner U, Budny T et al. 2014. Clinical benefit and improvement of activity level after reconstruction surgery of Charcot feet using external fixation: 24-months results of 292 feet.BMC Muscoloskeletal Disorders, 15:392.
- Liu G 2008. Is External Fixation Overutilized In Managing Charcot In The Diabetic Foot? Podiatry Today; 21(2):1-6