Early Charcot Foot Diagnosis is essential to a proper management, but this can be challenging. There are some factors that should increase clinical suspicion for acute Charcot arthropathy, namely if the patient presents with:
- Type 1 or 2 diabetes
- Minimal or no foot pain (in most cases)
- No suspicion for infection
- Obesity
- Unilateral edematous, erythematous, warm limb with no open wounds
- Peripheral neuropathy of any etiology
- Increased tracer (radionuclide) uptake in bone scans
- Negative labelled white cell scans (In-WBC)
Imaging tools play a central role in the early and accurate diagnosis of Charcot Foot and Ankle, to distinguish it from osteomyelitis, and to monitor the disease progression and complications. The imaging techniques currently in use for the evaluation of Charcot arthropathy are conventional radiography, computed tomography, nuclear medicine scintigraphy (radionuclide scanning), magnetic resonance imaging, and positron emission tomography.
In this article, we will explore how radionuclide imaging can be used in the context of Charcot Foot and Ankle.
The Role of Nuclear Medicine
The use of nuclear medicine to perform bone scans with small amounts of radioactive tracers (radionuclides) is valuable to have a functional method of diagnosis, as opposed to the purely anatomical methods offered by other imaging tools.
The most widely used radionuclide study for the evaluation of Charcot Foot and Ankle is the bone scintigraphy. This imaging technique can exclude osseous disease in a patient with low clinical suspicion of osteomyelitis and no signs of Charcot Joint on plain radiographs.
The traditional 99technetium bone scan has three imaging phases: blood flow, blood pool, and delayed phases. When acute Charcot arthropathy is present, there is an increased tracer uptake to the affected joint in all three phases of a bone scan. The addition of a fourth phase 24 hours later seems to enhance the specificity of the technique, as tracer uptake in woven bone continues for a longer period of time.
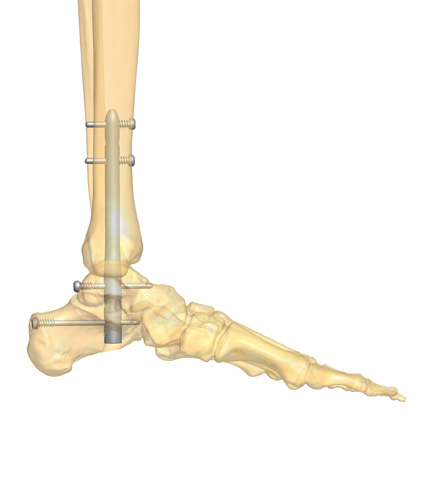
The use of nuclear medicine imaging is generally the preferred method when the patient has orthopedic hardware in the foot and ankle. It is worth noting that the presence of diffuse or regional ischemia can result in false-negative nuclear images. In those cases, the use of MRI is favored.
Keeping the Patients Involved
The main challenge when making a Charcot Foot diagnosis is to distinguish the early signs from other inflammatory conditions. A delay in the diagnosis and treatment may lead to dramatic consequences, including foot deformity, ulceration, infection, and – in a worst-case scenario – to limb amputation.
Imaging plays a pivotal role in arriving at the definitive diagnosis of Charcot Foot and Ankle, and a qualified radiologist can correctly distinguish the signs of osteomyelitis from a neuropathic arthropathy.
Patients should play an active role in the management of their condition. If they are aware of Charcot Foot symptoms, appropriately care for their feet, and quickly report any alterations to a member of their multidisciplinary healthcare team, their outcomes can be greatly improved. The current clinical evidence regarding better outcomes that can be achieved with the multidisciplinary approach are only relevant if the patient assumes his or her key role.
If you would like some information to give your patients regarding Charcot Foot and Ankle, we suggest downloading the Patient Informative Cards “Stand On Your Feet: A Program of Empowerment for Your Diabetic Foot Management.“

References
- Capobianco CM et al. J Orthop Surg Res. 2010 Feb 11;5:7.
- Mautone M, Naidoo P. J Med Imaging Radiat Oncol 2015 Aug;59(4):395-402.
- Wang A et al. Burns Trauma. 2020 Jul 6;8:tkaa017.
- Schoots et al Semin Musculoskelet Radiol. 2010 Sep;14(3):365-76.
- Marmolejo VS et al. Am Fam Physician. 2018 May 1;97(9):594-599.
- Rogers LC, Bevilacqua NJ. Clin Podiatr Med Surg 2008 Apr;25(2):263-74, vii.
- Marmolejo VS et al. Am Fam Physician. 2018 May 1;97(9):594-599.
- Ergen FB et al. Diabet Foot Ankle. 2013 Nov 20;4.