The successful treatment of Charcot foot does not end with a completed surgery; success also requires a diligent postoperative care regime. This devastating condition mainly affects patients with diabetes and peripheral neuropathy, resulting in bone destruction and joint deformation1. During the initial, inflammatory stage, the recommended treatment consists of off-loading with total contact casts or custom orthotics to prevent further damage, although surgical management is indicated in cases of severe instability or soft tissue compromise2. After the acute stage, the focus of treatment is on deformity correction and foot reconstruction to prevent further damage and improve the patients’ quality of life2.
In this article, we will review the aspects involved in Charcot foot reconstruction and how to optimize the postoperative management to improve success rates and outcomes.
Post-Surgical Management
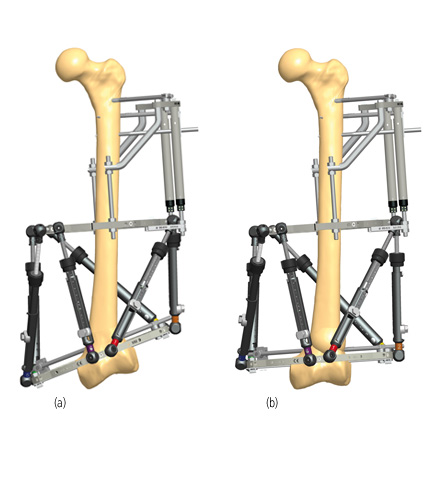
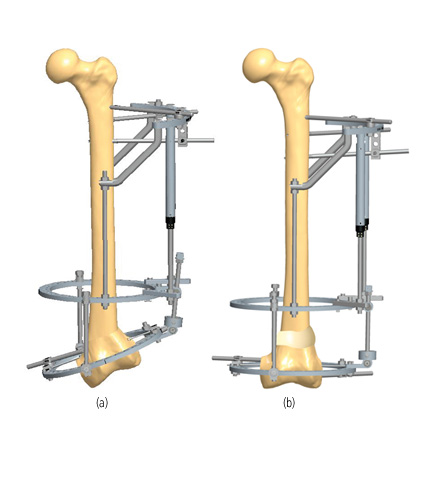
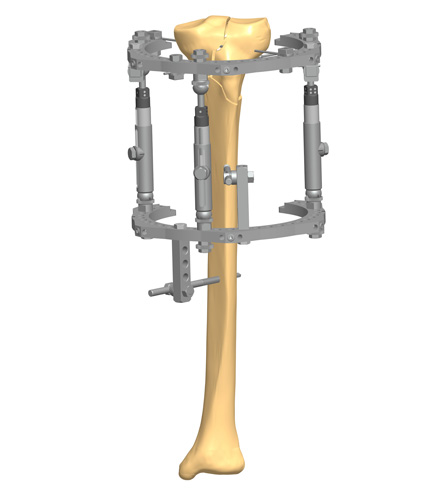
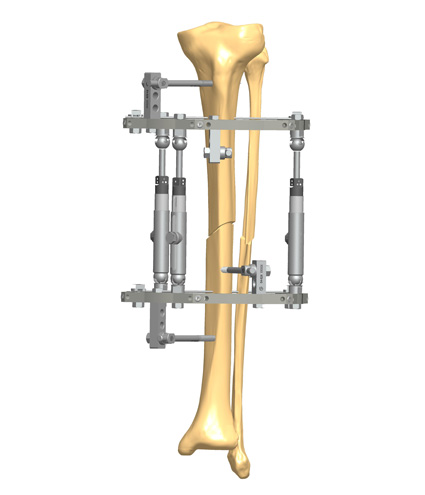
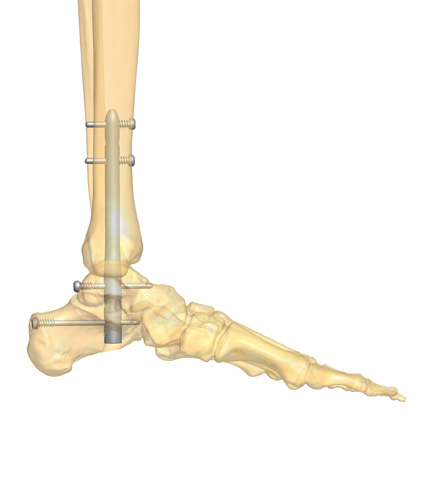
Surgical reconstruction of a Charcot foot can be obtained with internal or external fixation devices, and sometimes both are used (hybrid fixation), according to the level and location of the deformity3.
Postoperative management and rehabilitation often require extensive resources and patient diligence, particularly with more extensive surgeries4.
Complication rates after surgery can be high, with Ha and colleagues reporting an overall complication rate of 36% in their systematic review5. Further analysis showed that external fixation was associated with a complication rate of 25%, while internal fixation had a complication rate of 41.4%. The use of combined internal and external fixation was associated with the highest complication rate, which occurred in 70% of patients. However, the author noted that the low number of patients undergoing hybrid fixation precluded definitive conclusions.
Circular fixation is associated with a high incidence of pin site infections, for which a careful postoperative care routine is advised5. Pin site care should be done every day, using a clean swab soaked with saline or a cleaning solution to remove any drainage or debris, followed by a dry swab. Each swab should be used on a single pin site. This video explains the process of pin site care.
Complications associated with internal fixation include deep infection, major hardware failure, unstable nonunion, and wound dehiscence6.
A low number of patients undergo reconstruction with combined internal and external fixation, possibly because it is usually reserved for those with poor quality bone or when immobilization is not possible7. Complications from combined internal and external fixation include wound dehiscence, pin site infection, and superficial wound infection7.
“Charcot patients are the most challenging patients: the risk for infection is much higher; most of them are diabetic; and the risk for nonunion is also much higher. In addition, patients must tolerate non-weightbearing for about 3 months, unless they are treated with a frame.” – Dr. Daniel Scott, Medical University of South Carolina (MUSC) Orthopaedics, Charleston
Post-operatively, the operated limb should remain elevated for 48 hours and antibiotics administered according to the preoperative microbiological culture and sensitivities8. Antibiotics can be altered if the results from the intraoperative microbiological culture require it8. The surgical wound is inspected 2 days after surgery, and the suction drain (if any was used) is removed8.
The most important aspect of post-surgical management is complete off-loading and non-weightbearing4,8-10. Once swelling in the foot has decreased, the leg is placed in a total contact cast and the patient is strictly prohibited from weightbearing for a period that can range from 6 to 16 weeks, until signs of bony union are confirmed radiologically4,8,9. It is important to be careful not to overload the contralateral unaffected foot during this period9.
“Patients treated with a frame require follow-up every 2 weeks to monitor pin site infections or detect any complications with the frame. Less frequent visits are required after frame removal when patients ambulate with a walking cast or boot. For internal fixation, sutures are usually removed after 2 weeks, which is followed by monthly visits.” – Dr. Daniel Scott, Medical University of South Carolina (MUSC) Orthopedics, Charleston.
Sometimes, it is this prolonged time of immobilization that can heavily impact outcomes, so it is essential to ensure that the patient has the adequate environmental and social resources to adhere to complete non-weightbearing after Charcot foot surgery4. Dr Lisa Grant-McDonald, DPM, notes that all Charcot patients want to start weightbearing as soon as possible but if started too soon, weightbearing can lead to nonunion, especially in complex midfoot cases of Charcot foot.
Partial weightbearing is allowed after the first signs of radiological union are observed, but always carefully monitored for signs of implant failure or loss of correction8. When there is radiological evidence of complete bone union, the patient is allowed to mobilize without weightbearing restrictions, either using custom-made orthotics or diabetic shoes8.
Difficulties When Managing Diabetic Patients
Ideally, every collapsed or deformed Charcot foot would be surgically restored, resulting in a biomechanically sound and ambulatory foot4. However, not all patients have the necessary requirements to endure the surgery itself, but also to comply and be adequately supported in the postoperative period.
Patients with diabetes present unique challenges for Charcot foot reconstruction, because anesthesia and surgical stress result in metabolic perturbations that can change normal glucose homeostasis11. Postoperative hyperglycemia is a risk factor for sepsis and impaired healing, while unmanaged hypoglycemia may result in several neurological complications, including somnolence, unconsciousness, and seizures11.
The foundation of good postoperative care in diabetic patients is based on careful blood glucose monitoring, with a goal of 80-150 mg/dL, although the optimal range remains controversial. It is worth noting that even if a type 2 diabetic patient had adequate preoperative glycemic control with diet and oral medications, they may require insulin in the postoperative period to counteract glycemic imbalances caused by surgical stress12.
The presence of diabetes in a patient with Charcot foot may dictate the approach to surgical reconstruction. According to Dr Mohammad Sharif, DPM, talus reconstruction should be avoided in patients with diabetes, given the potential for worse outcomes; tibiocalcaneal fusion is the preferred option in this patient population.
Patients with diabetes have an increased risk of Charcot recurrence after acute treatment, up to 17% in the same foot13. In addition, there is an increased risk for the development of Charcot in the contralateral foot, highlighting the importance of continued surveillance of at-risk patients. With timely diagnosis and appropriate treatment, it is possible to prevent 4 out of 5 amputations. This means more than limb salvage, since more advanced reconstruction techniques allow the achievement of independent ambulation with commercially available therapeutic footwear, which improves patients’ quality of life14.
Further Reading
There are many aspects to consider in the preoperative assessment of a patient with Charcot foot, including deformity characteristics, patient characteristics, and the ability to endure a long recovery period. Surgical management of a Charcot foot has the goal of obtaining a plantigrade, ulcer-free foot that can bear weight, but it is hindered by high complication rates that can ultimately lead to treatment failure. Performing the appropriate postoperative treatment is critical in ensuring successful surgical outcomes and, therefore, is an area to which surgeons should pay close attention.
To learn more about postoperative management following Charcot foot reconstruction surgery, please read our “Charcot Foot Reconstruction Case Reports,” available to subscribers/registered users.

References
- Dardari D. An overview of Charcot’s neuroarthropathy. J Clin Transl Endocrinol. Dec 2020;22:100239. doi:10.1016/j.jcte.2020.1002391.
- Stuto AC, Stapleton JJ. Surgical Considerations for the Acute and Chronic Charcot Neuroarthropathy of the Foot and Ankle. Clinics in Podiatric Medicine and Surgery. 2022/04/01/ 2022;39(2):331-341. doi:https://doi.org/10.1016/j.cpm.2021.11.005
- Abyar E, McKissack H, Johnson MD. Chapter 19 – The surgical management of the Charcot foot: physical examination of the foot prior to surgery, indications and criteria for amputation, and surgical techniques. In: Pierre-Jerome C, ed. The Essentials of Charcot Neuroarthropathy. Elsevier; 2022:441-448.
- Chen S, Miller JD, Steinberg JS. Management of the Charcot Foot and Ankle: Nonreconstructive Surgery. Clinics in Podiatric Medicine and Surgery. 2022/10/01/ 2022;39(4):559-570. doi:https://doi.org/10.1016/j.cpm.2022.05.003
- Ha J, Hester T, Foley R, et al. Charcot foot reconstruction outcomes: A systematic review. J Clin Orthop Trauma. May-Jun 2020;11(3):357-368. doi:10.1016/j.jcot.2020.03.025
- Trepman E, Nihal A, Pinzur MS. Current Topics Review: Charcot Neuroarthropathy of the Foot and Ankle. Foot & Ankle International. 2005/01/01 2005;26(1):46-63. doi:10.1177/107110070502600109
- Hegewald KW, Wilder ML, Chappell TM, Hutchinson BL. Combined Internal and External Fixation for Diabetic Charcot Reconstruction: A Retrospective Case Series. The Journal of Foot and Ankle Surgery. 2016/05/01/ 2016;55(3):619-627. doi:https://doi.org/10.1053/j.jfas.2015.04.016
- Kavarthapu V, Vris A. Charcot midfoot reconstruction—surgical technique based on deformity patterns. Annals of Joint. 2020;5
- Nsubuga MJ, Pierre-Jerome C. Chapter 21 – The surgical approach and follow-up of the complicated Charcot foot: general considerations. In: Pierre-Jerome C, ed. The Essentials of Charcot Neuroarthropathy. Elsevier; 2022:455-471.
- Miller R. NEMISIS: Neuropathic Minimally Invasive Surgeries. Charcot Midfoot Reconstruction, Surgical Technique, Pearls and Pitfalls. Foot and Ankle Clinics. 2022/09/01/ 2022;27(3):567-581. doi:https://doi.org/10.1016/j.fcl.2022.05.001
- Sudhakaran S, Surani SR. Guidelines for Perioperative Management of the Diabetic Patient. Surgery Research and Practice. 2015/05/19 2015;2015:284063. doi:10.1155/2015/284063
- Hoogwerf BJ. POSTOPERATIVE MANAGEMENT OF THE DIABETIC PATIENT. Medical Clinics of North America. 2001/09/01/ 2001;85(5):1213-1228. doi:https://doi.org/10.1016/S0025-7125(05)70373-4
- Jansen RB, Jørgensen B, Holstein PE, Møller KK, Svendsen OL. Mortality and complications after treatment of acute diabetic Charcot foot. Journal of Diabetes and its Complications. 2018/12/01/ 2018;32(12):1141-1147. doi:https://doi.org/10.1016/j.jdiacomp.2018.09.013
- Pinzur MS, Schiff AP. Deformity and Clinical Outcomes Following Operative Correction of Charcot Foot: A New Classification With Implications for Treatment. Foot Ankle Int. Mar 2018;39(3):265-270. doi:10.1177/1071100717742371