Appropriate timing for surgical intervention is a matter of controversy among specialists1. While in the past Charcot foot surgical reconstruction was mainly reserved to salvage the limb, today surgeons also perform operative corrections to ensure patients can use commercially available footwear instead of cumbersome orthoses1. Regardless, the main goal of Charcot foot surgery, independent of the fixation method, is to create a stable and plantigrade foot. This article will discuss different approaches for Charcot foot surgery with internal fixation, focusing on midfoot reconstruction.
Challenges of Midfoot Pathologies
For many surgeons, Charcot reconstruction of the midfoot is more challenging than hindfoot pathologies.
This is also confirmed by Lisa Grant-McDonald (DPM, Doctors Grant Foot & Ankle, Virginia Beach): “Getting a dislocated Lisfranc joint back in the right direction with olives [using external fixation] can be really challenging. In addition, achieving an almost perfect stabilization is much more important than for the hindfoot. Hindfoot pathologies are more straightforward and usually achieve good results.”
Midfoot Reconstruction with Beams
Beaming is an increasingly used intramedullary reconstruction method for midfoot pathologies, as it realigns the anatomy and reinforces the corrected foot at the same time2. Large-diameter cannulated screws or bolts are placed in the medullary canal of one or more midfoot columns2. Drs. William Grant and Lisa Grant-McDonald describe the following beaming approach2:
- Achilles tendon lengthening: Contracture of the Achilles tendon can worsen midfoot collapse and increases forefoot stress due to negative calcaneal inclination angles. Achilles tendon lengthening is therefore recommended to reduce the risk of hardware failure. The main approaches for Achilles tendon lengthening are the open approach (incision at the medial border of the mid-substance of the tendon) or the percutaneous approach using a “Z” cut for lengthening.
- Hindfoot pinning: Hindfoot stabilization with a Steinmann pin is recommended to place the ankle in a neutral position and the calcaneus in a positive inclination angle.
- Midfoot osteotomy:
- Any dislocated bone and articular cartilage should be removed.
- Bony structures involved in the collapse can now be prepared for fusion. The Lisfranc and talonavicular joint are frequently involved in the medial aspect. A lateral incision is usually required to reduce the cuboid, which is often dislocated at the calcaneocuboid joint and the cuboid metatarsal articulation.
- Once the midfoot is de-rotated against a stable hindfoot block, the midfoot can then be fixated.
- Hardware application:
- Placement of both a medial and lateral beam can prevent recurrent midfoot deformity.
- Supplemental beams should be considered to achieve better postoperative outcomes. A beaming “Truss” creates a functional triangle by crossing the base of one metatarsal of the medial column and the body of the calcaneus.
Lisa Grant-McDonald (DPM, Doctors Grant Foot & Ankle, Virginia Beach) provides insights into her beaming approach: “My beaming approach usually starts with Achilles tendon lengthening and extra articular pinning of the hindfoot into neutrality. A medial Beam wire is placed first from the 1st metatarsal head back to the body of the talus. At this time the foot is derotated and the cuboid is lifted from its typically dislocated position. The lateral column is pinned and a beam wire is placed from between the 4th and 5th metatarsal into the central aspect of the CC joint. Next the subtalar joint wire is applied followed by a final “Truss” beam locking the 2nd metatarsal base to the anterior process of the calcaneus. Once ‘weight bearing’ alignment is confirmed with radiographs each beam is applied in the same order.”
There are challenging situations for beaming, especially in patients with soft tissue contractures of the midfoot, as Stephanie Oexeman (DPM, Oexeman Foot & Ankle, Chicago) explains: “Proper alignment of the midfoot can be difficult. It is important to take enough time and be patient. Inadequate intraoperative alignment won’t get better later on!”
Beam failure can occur due to weak implant material, insufficient sizing, or inappropriate screw configuration2. Stainless steel is the preferred material for Charcot foot surgery2 due to the superior biomechanical properties of stainless steel, including higher stiffness, force to failure, and pullout strength3. The main benefits of beaming the midfoot are that it preserves soft tissue and provides a superconstruct without extensive soft tissue dissection2. However, reported hardware failure rates vary significantly from 4% to 67%4-6. Surgeons should also be aware of the risk for deep infection in the presence of full-thickness plantar ulcers4.
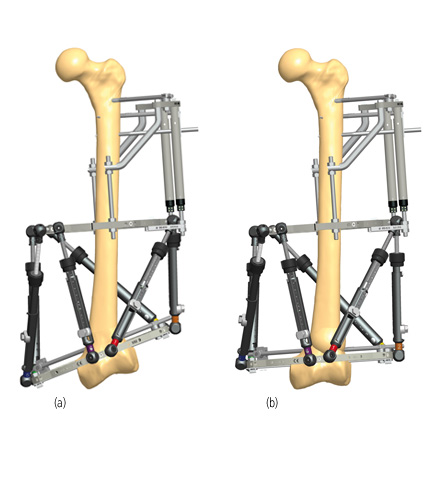
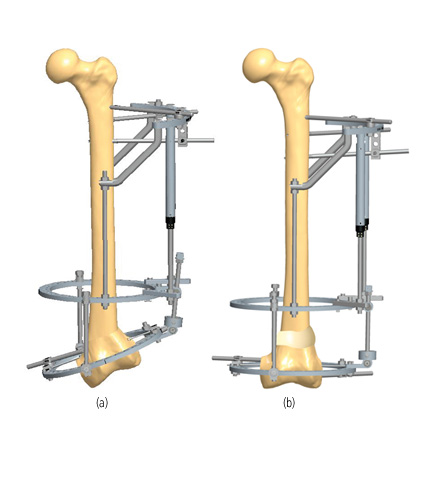
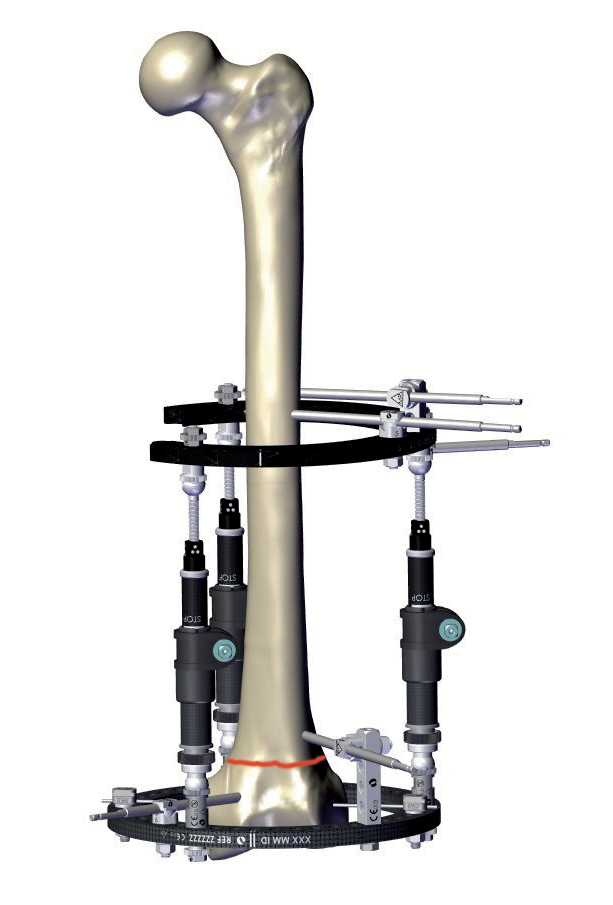
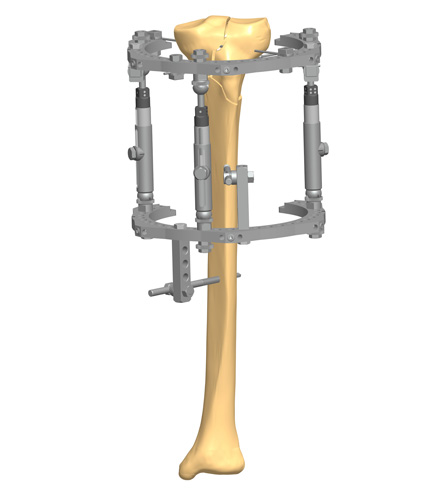
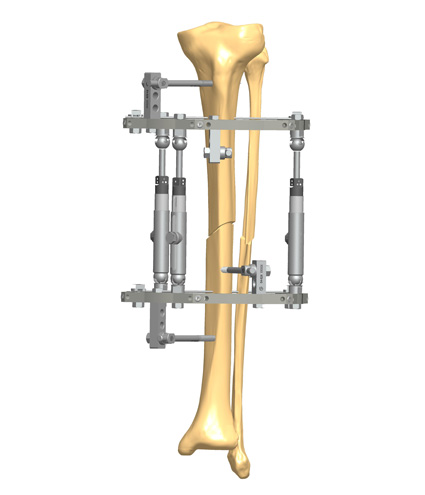
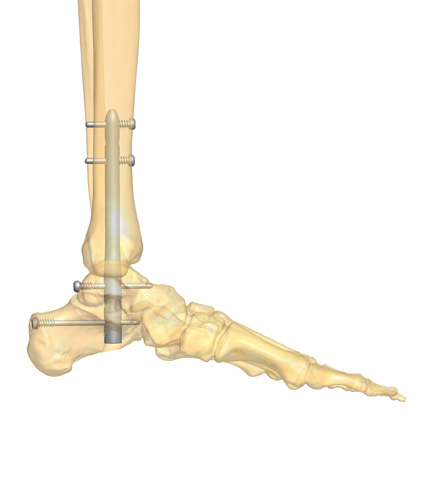
Figure 1 shows an example case where beaming of the medial column, lateral column, and subtalar joint were performed along with an Achilles tendon lengthening. In addition, a trussing technique was used where a “truss” beam was placed between the medial and lateral columns in the midfoot.

Midfoot Reconstruction with Medial Column Plates
The reduction and fixation of the medial column are key elements in treating midfoot deformities7. Medial column fusion has become a common technique that can also be considered for earlier stages of Charcot arthropathy8. However, standard implants and reconstruction techniques for midfoot arthrodesis in severe deformities can frequently lead to high complication rates due to loss of fixation8,9. Modern fixation techniques, including superconstructs, maximize stability as they fuse beyond the zone of injury9. Superconstructs utilize two or more devices for fixation and enhanced stability such as a medial column plate positioned over a beam.
The principle of superconstructs was first described by Sammarco et al. (2009) and is defined by four factors8:
- Fusion is extended to non-affected joints for better fixation
- Bone resection to shorten the extremity is performed to allow adequate reduction without undue tension on the soft tissue envelope
- The strongest implant, as tolerated by the soft tissue envelope, is selected
- Implants are positioned in a way to maximize mechanical integrity.
Superconstruct techniques have evolved for several reasons. Charcot foot surgery is complicated by sensory neuropathy and the inability to avoid weightbearing and the dissolution of bone, including resorption and fragmentation9. Therefore, the poor quality of the bone can make fixation in this area almost impossible9. Superconstructs bypass this problem by using non-affected bone for fixation9.
Locking plates are frequently used devices for medial column plating as they create a strong fixed-angle device and provide the ability to include multiple bone fragments into the fusion mass9. Plates with high strength are recommended to resist cycle loading as soon as patients start weightbearing9.
Considerations for Postoperative Care
The best postoperative care is discussed controversially, especially regarding immobilization. Experts consider long-term bracing or casting from 3 to 7 months as a key to achieving successful outcomes10. Alrashidi et al. also recommended keeping the affected limb elevated for the first days to reduce edema, prescribing deep vein thrombosis prophylaxis, and regularly checking the vascular status7. Physiotherapy can be started after removal of the stitches with regular stretching of the Achilles tendon to prevent recurrent contracture7. Routine radiographs should be considered at 6 weeks, 3 months, and every 6 months until bone union is clearly evident7.
Further Reading
Download the Charcot foot surgical cases available for more information about internal fixation for midfoot reconstruction.

References
1. Pinzur MS, Schiff AP. Deformity and Clinical Outcomes Following Operative Correction of Charcot Foot: A New Classification With Implications for Treatment. Foot Ankle Int. Mar 2018;39(3):265-270. doi:10.1177/1071100717742371
2. Grant W, Grant-McDonald L. Beaming the Charcot Foot. Clin Podiatr Med Surg. Oct 2022;39(4):605-627. doi:10.1016/j.cpm.2022.05.007
3. Wukich DK, Liu GT, Raspovic K, Vicenzi F. Biomechanical Performance of Charcot-Specific Implants. J Foot Ankle Surg. May-Jun 2021;60(3):440-447. doi:10.1053/j.jfas.2020.05.016
4. Ford SE, Cohen BE, Davis WH, Jones CP. Clinical Outcomes and Complications of Midfoot Charcot Reconstruction With Intramedullary Beaming. Foot Ankle Int. Jan 2019;40(1):18-23. doi:10.1177/1071100718799966
5. Grant WP, Garcia-Lavin S, Sabo R. Beaming the columns for Charcot diabetic foot reconstruction: a retrospective analysis. J Foot Ankle Surg. Mar-Apr 2011;50(2):182-9. doi:10.1053/j.jfas.2010.12.002
6. Butt DA, Hester T, Bilal A, Edmonds M, Kavarthapu V. The medial column Synthes Midfoot Fusion Bolt is associated with unacceptable rates of failure in corrective fusion for Charcot deformity: Results from a consecutive case series. Bone Joint J. Jun 2015;97-b(6):809-13. doi:10.1302/0301-620x.97b6.34844
7. Alrashidi Y, Hügle T, Wiewiorski M, Herrera-Perez M, Valderrabano V. Surgical Treatment Options for the Diabetic Charcot Midfoot Deformity. Clin Podiatr Med Surg. Jan 2017;34(1):43-51. doi:10.1016/j.cpm.2016.07.006
8. Sammarco VJ. Superconstructs in the treatment of charcot foot deformity: plantar plating, locked plating, and axial screw fixation. Foot Ankle Clin. Sep 2009;14(3):393-407. doi:10.1016/j.fcl.2009.04.004
9. Sammarco VJ, Chevillet J. The role of internal fixation in surgery of the Charcot foot and the evolution of “super- construct” techniques. Current Orthopaedic Practice. 2010;21(3)
10. Salvaterra P. The Surgical Management of Neuropathic (Charcot) Foot – A Practical Guideline. 2017;