It is known that around 9 per cent of patients with diabetic neuropathy and foot ulcers develop a Charcot foot and ankle. This pathology often goes unrecognized, particularly during the acute phase, until severe complications occur, such as an abnormal pressure distribution on the plantar fascia with bones weakened enough to fracture, followed by a marked foot and ankle deformation and, in the worst cases, by amputation. Thus, today, one of the most crucial questions is how to timely diagnose this condition.
The acute phase of Charcot foot and ankle can be easily misdiagnosed, most often as cellulitis, gout, deep thrombosis or a sprain. Being associated with multifactorial risk factors, it needs a concerted effort from a multidisciplinary team.
If untreated, this destructive process may lead to fracture, rigid foot deformities – the well-known rocker bottom foot – and at worst to the loss of a toe, a foot, a leg, or life itself. Limb salvage is of paramount importance as the contralateral foot may be at risk for Charcot neuroarthropathy and, if the other side becomes involved, the patient might end up with bilateral amputation.(1)
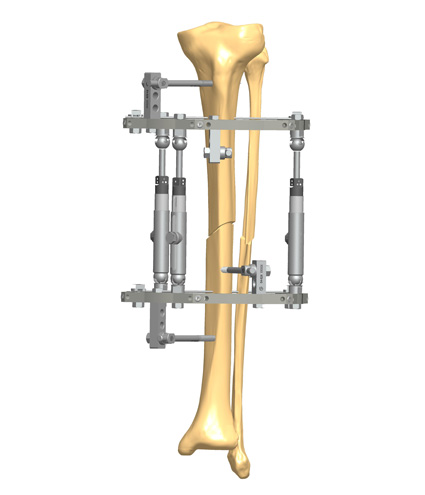
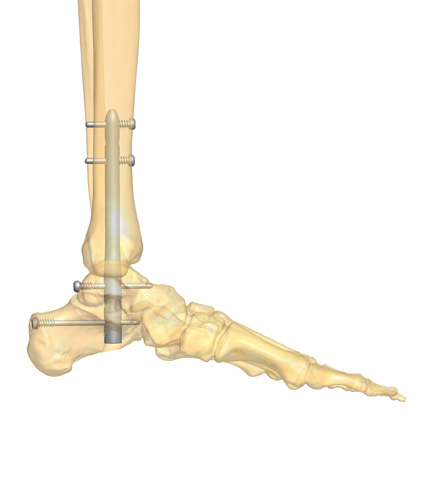
This disease can be treated with physical therapy, braces or casting, pain medication, off-loading and surgery. Appropriate surgical management, with the use of internal and/or external fixation, can help to reverse bone and joint deformities and save the foot.
Timely and correct clinical diagnosis in the primary care setting facilitates treatment, decreases long-term disability and may prevent amputation. The best safeguard is a high index of suspicion, especially in any diabetic patient older than 40 years, obese, with a swollen, red, warm foot, in the presence of somatic or sympathetic autonomic neuropathy. Even with normal radiography, MRI or computed tomography should be performed.(2) Once treatment begins, imaging is performed periodically to evaluate the evolving status of the condition.(3)
During the patient’s physical examination, the doctor should look for hot, red, swelling foot or ankle (the Charcot active phase); higher temperature of 2° C or 4° F of one foot compared with the contralateral one; interdigital maceration; skin lesions, foot ulcers and open wounds; hypertrophic calluses or corns; discolored, ingrown nails; crepitant cellulitis, fungal infection; loss of foot or limb sensitivity; bone deformities; limited range of joint motion; absence of Achilles Tendon reflex; vascular compromise, with sudden absence of dorsalis pedis and posterior tibial pulses; and peripheral arterial disease. He or she should know about the patient’s history – diabetes and prior diabetic foot problems(4), a prior angioplasty, stent or leg bypass surgery, traumas, smoking, alcohol abuse, physical activity.
References
- https://www.foothealthfacts.org/conditions/charcot-foot
- Cavanagh PR, Young MJ et al.1994. Radiographic abnormalities in the feet of patients with diabetic neuropathy. Diabetes Care; 17:201-9.
- Marmolejo VS, Arnold JF et al. 2018. Charcot Foot: Clinical Clues, Diagnostic Strategies, and Treatment Principles. Am Fam Physician; 97(9):549-99.
- Fauzi AA, Chung TY et al. 2016. Risk factors of diabetic foot Charcot arthropathy: a case-control study at a Malaysian tertiary care centre. Singapore Med J; 57(4):198-203.