When a bone breaks, all the systems work for the bone healing. Fracture healing is a natural, physiological process, and the surgeon may help nature to restore the biological, structural and mechanical properties of the bone as they were before the break, transforming the fracture into a healed, normal and straight bone.
Bone union is considered as the end point of fracture healing: the point at which the injured bone has recovered enough strength and stability to function as a weight-bearing structure without support.(1) There are some prerequisites for a successful healing, such as good blood supply at the fracture site, no soft-tissue interposition between the bone fragments, no major infection, and appropriate mechanical conditions for the different phases of the fracture healing process.
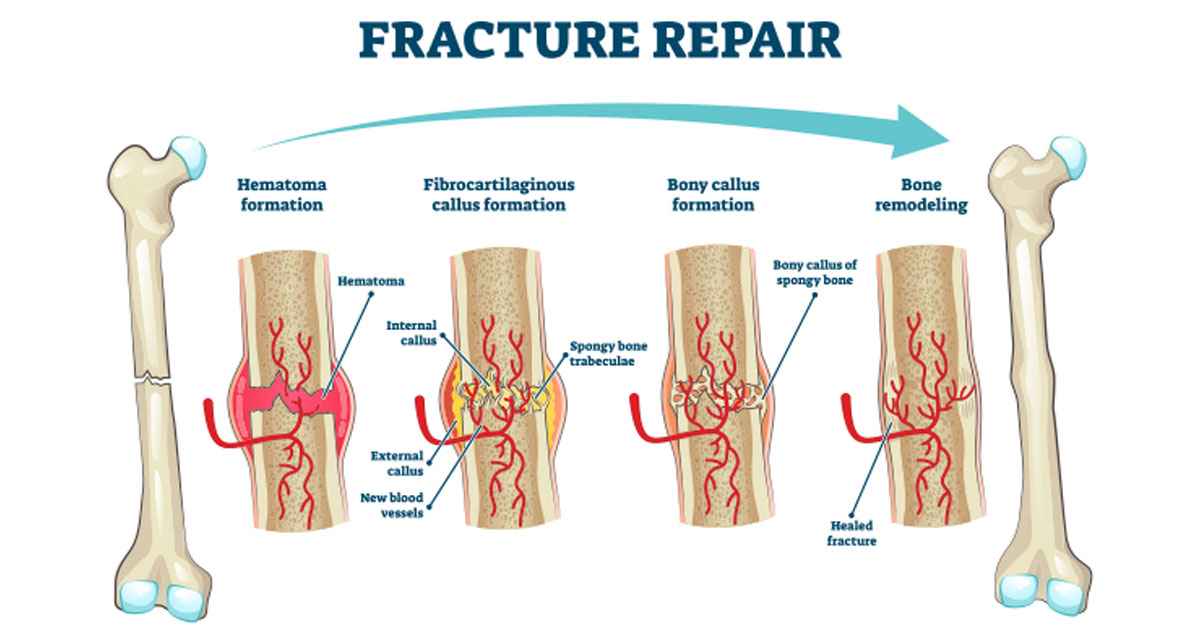
These phases are well known. During the initial inflammatory phase, there is formation of a hematoma at the injured site, with presence of inflammatory cells and granulation tissue which is the first callus response. In this first phase it is important to gain stability in order to maintain the hematoma’s integrity. Then soft callus and hard callus formations follows – the so called “reparative” and “modeling” phases. The last phase, starting around 6 weeks after the injury, is the “remodeling” one, in which the hard callus is replaced and remodeled into stronger lamellar bone by the action of osteoclast bone resorption and osteoblast bone formation.
Fracture healing is generally classified in two types, direct (primary) bone formation and indirect (secondary) healing or external callus formation. Direct healing is a slow process and occurs when the bony fragments are fixed together with compression. In this type of healing there is no callus formation, and the fracture ends are joined by osteoclast and osteoblast activity. Direct healing is seen after a very rigid stabilization, e.g. the one achieved with compression plating.
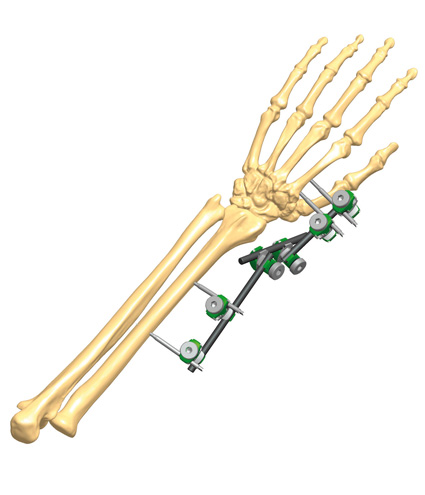
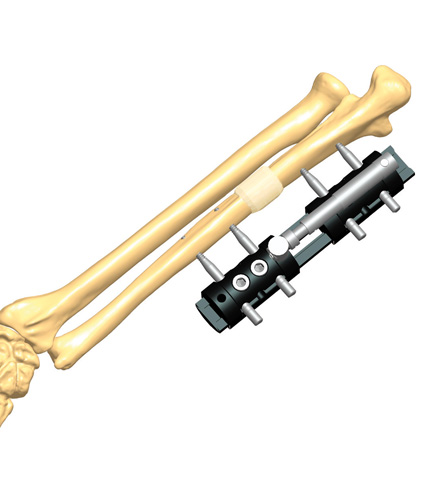
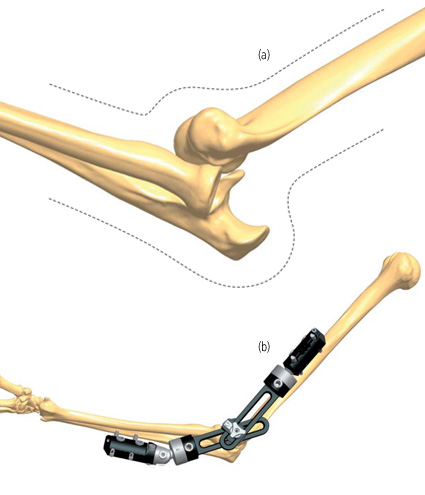
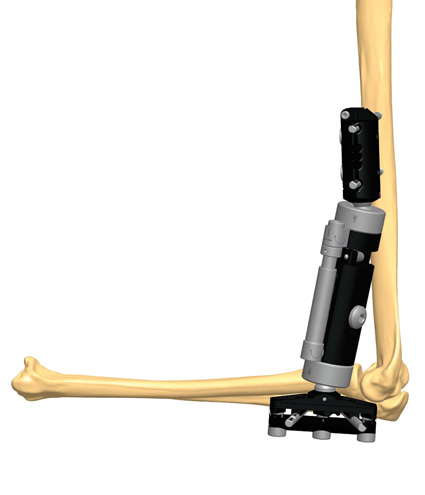
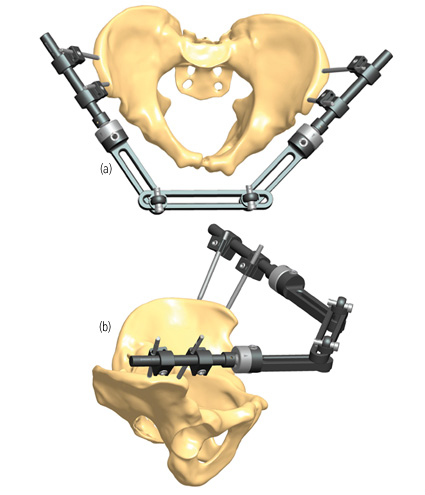
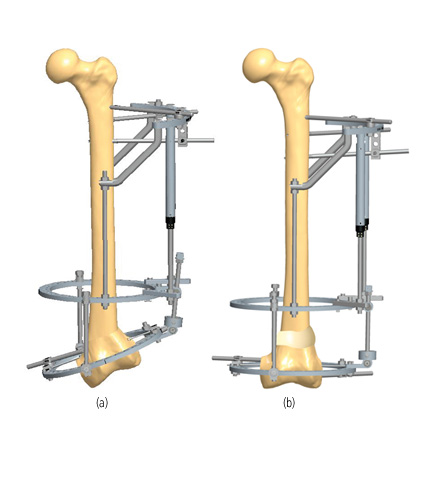
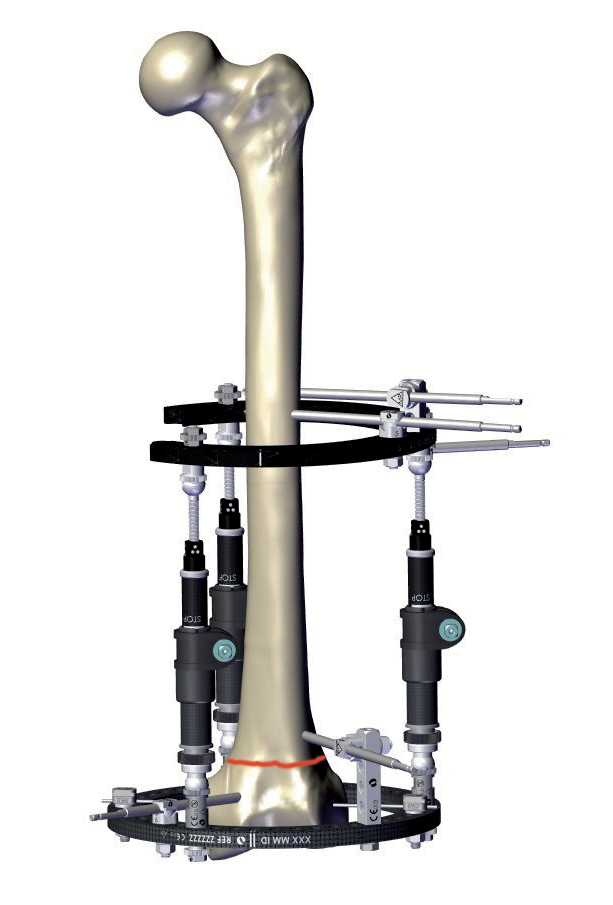
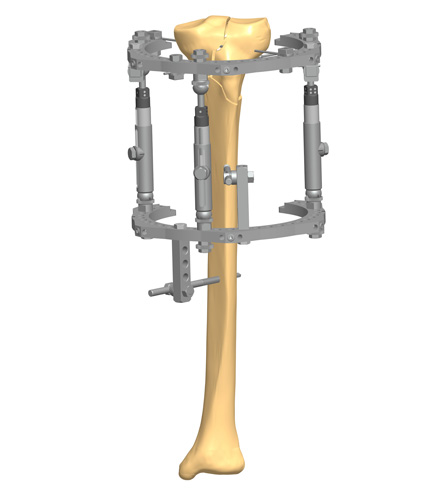
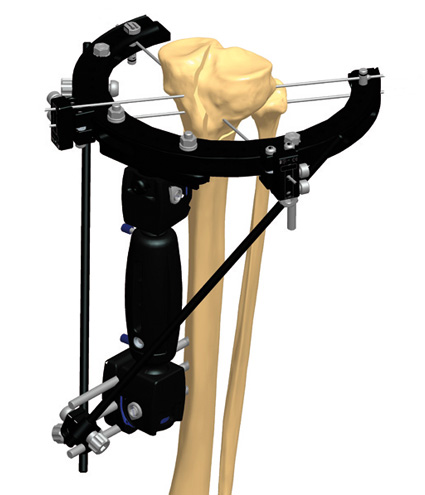
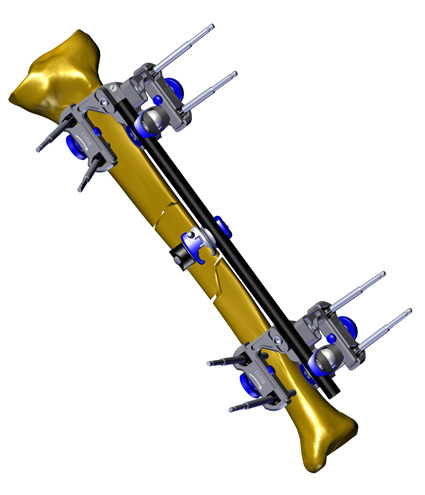
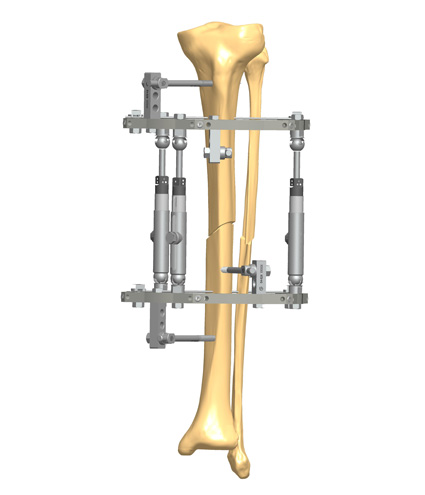
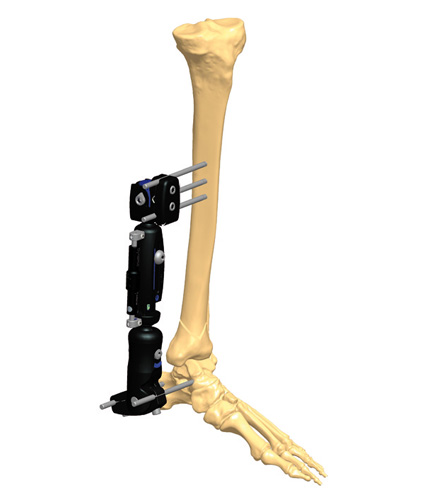
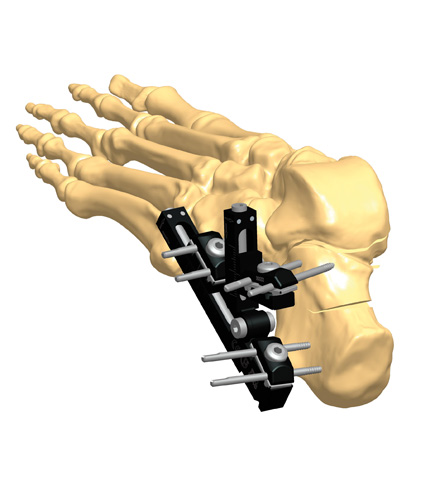
Indirect healing is more common, involving both endochondral and intramembranous bone healing.(2) It occurs when there is some motion at the fracture site, e.g. with intramedullary nailing, bridge plating or external fixation. The external callus is formed to reduce movement between the bone fragments, and while forming it provides strength and support to the healing bone.
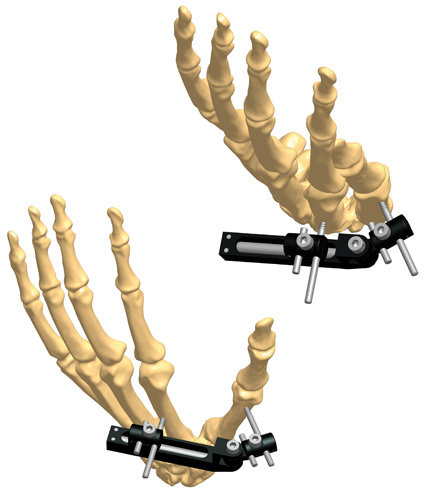
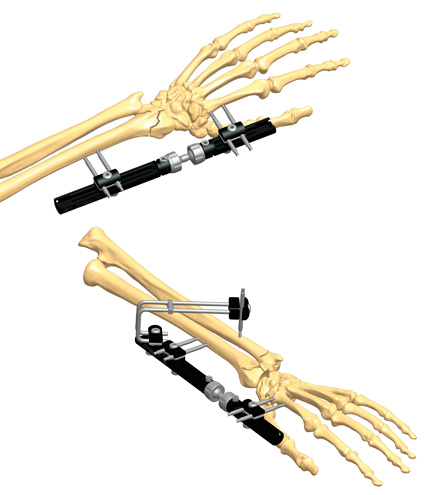
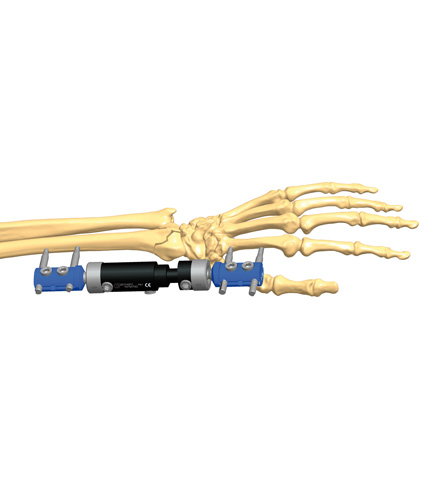
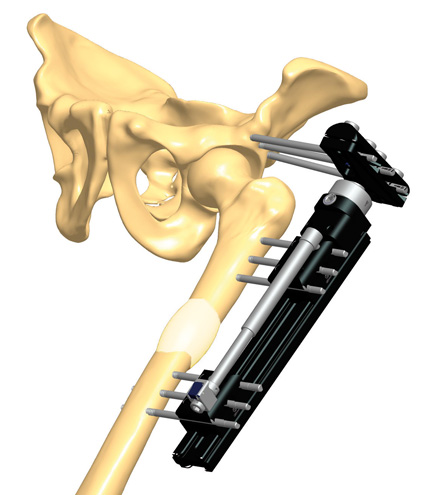
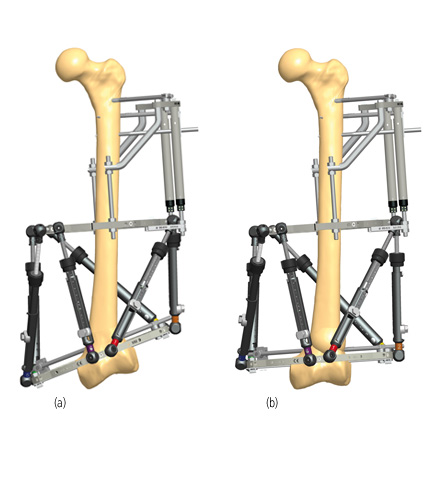
In the past, the use of external fixation was reserved for the most severe types of fracture. On the one hand, this was due to the type of devices available at the time – heavy, difficult and time consuming to apply. On the other hand, surgeons were worried about the risks of non union – eventually caused by excessive movement at the fracture site – and pin track infection. Nowadays it is recognized that external fixation allows small degrees of micromotion (dynamization), which promotes blood flow at the fracture site, and accelerates the bone healing process.(3)
References
- Marsh DR, Gang Li 1999. The biology of fracture healing: optimizing outcome. British Medical Bulletin; 55(4):856-69.
- Marsell R, Einhorn TA 2011. The biology of fracture healing. Injury; 42(6):551-5.
- Qi WC, Feng XR et al. 2020. The development and in vivo validation of an external fixation device with standardized micromotion for accelerating fracture healing. 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC); DOI:10.1109/EMBC44109.2020.9175437.