A typical question that a surgeon has to face when deciding the treatment of a bony injury is when to use internal fixation instead of external fixation. A common answer is “when the patient is compliant, with sufficient bone and soft tissue quality, and presents less complex fractures”. Surgeon’s expertise and preference may also affect the final surgical plan.
Every fixation method to manage fractures should be attentively evaluated on each individual clinical case: patient’s condition and age, type of fracture, mechanism of injury, and life style. The clinical experience of the surgeon, together with his/her preference, may also influence the decision making process. All of this information should lead to the most appropriate treatment. Some common techniques include:
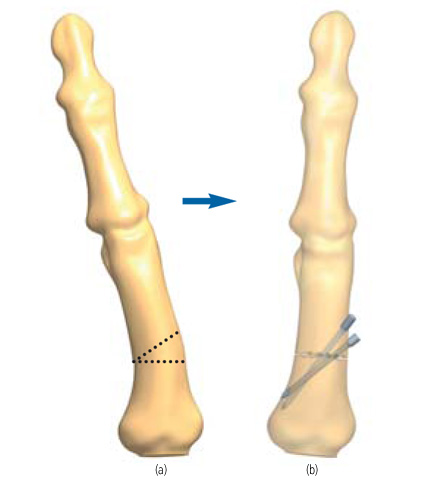
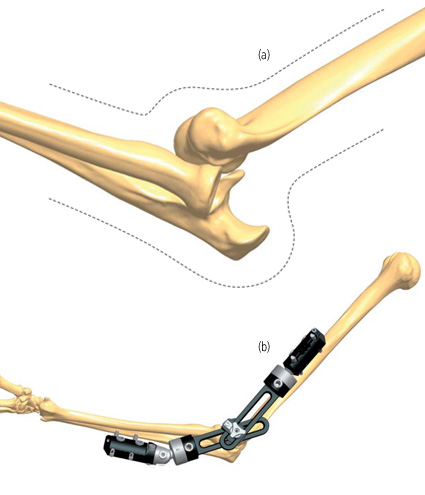
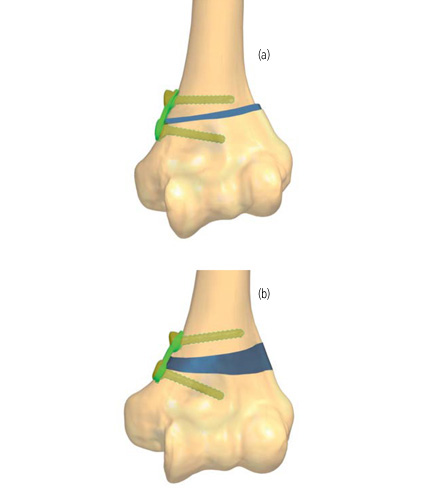
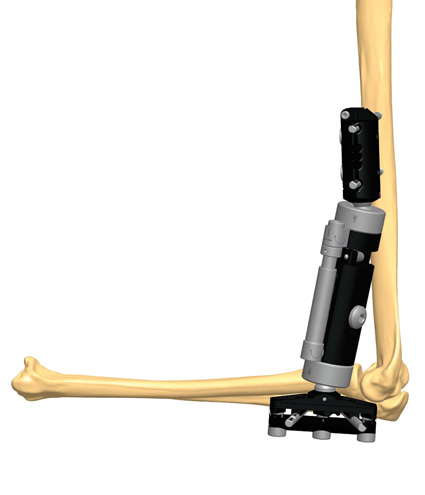
K-wires/Elastic Stable Intramedullary Nailing: especially when the patient is a child, and trauma regards the long bones, this is considered the gold standard of treatment. It is also indicated with obese patients. When inserting a wire near a joint, the wire must be placed in the end range of motion.(1)
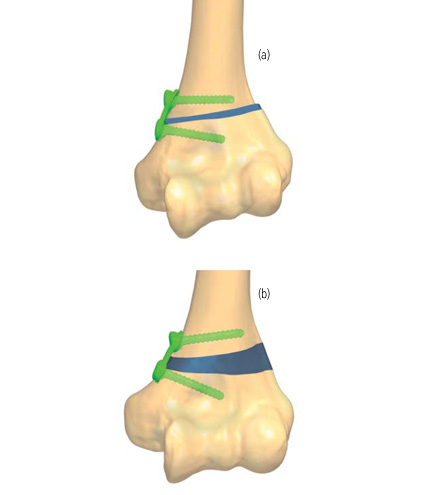
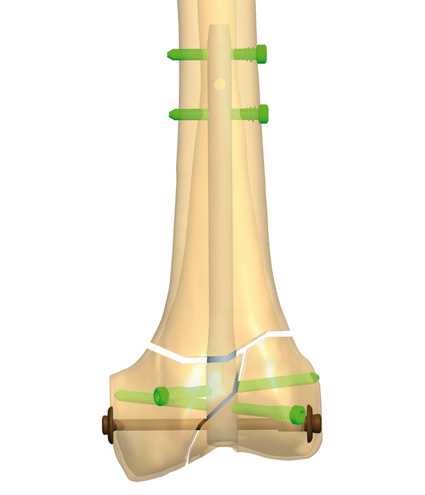
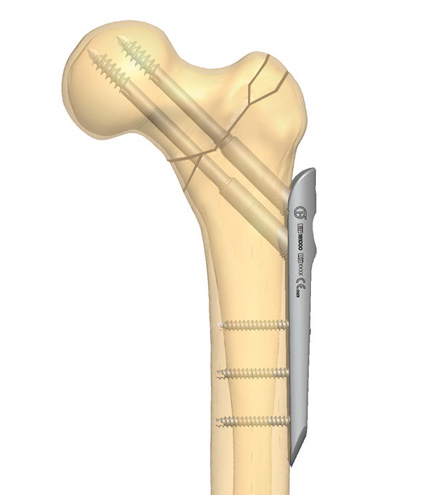
Open Reduction and Internal Fixation: when the patient is compliant, reliable, with sufficient bone quality and presents less complex fracture. It is indicated for the treatment of distal radial fractures.(2) The bones are reduced into their normal alignment and held together with screws, plates and/or an oblique tension band wire. Internal fixation may be contraindicated in the presence of an extremely severe comminution and soft tissue severe compromise.
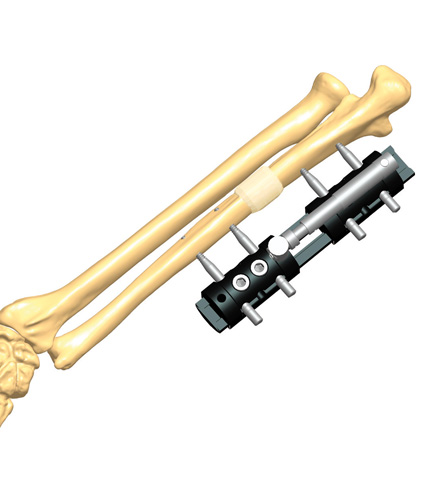
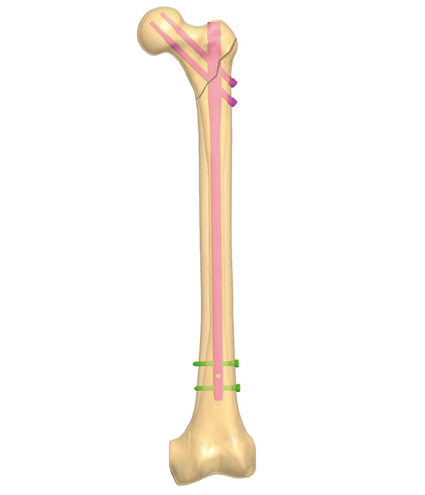
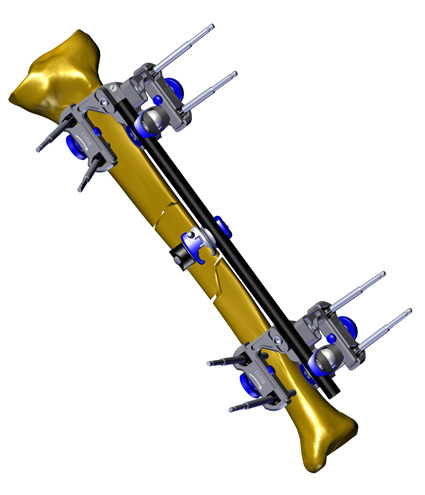
Intramedullary Rod fixation: it is generally applied with long bones/tibial fractures. It gives immediate stability and is minimally invasive.
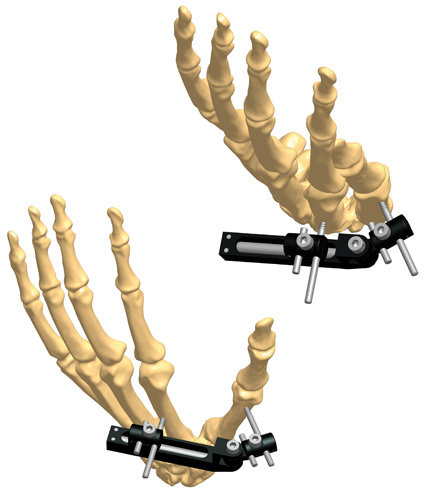
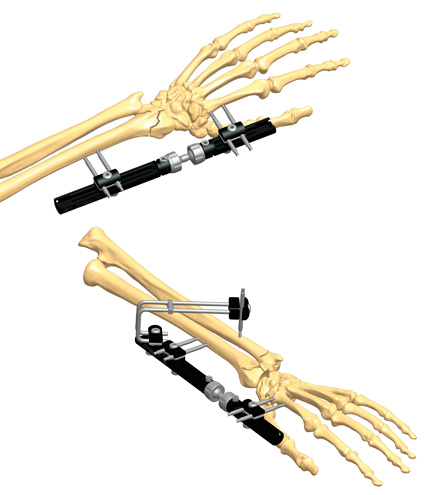
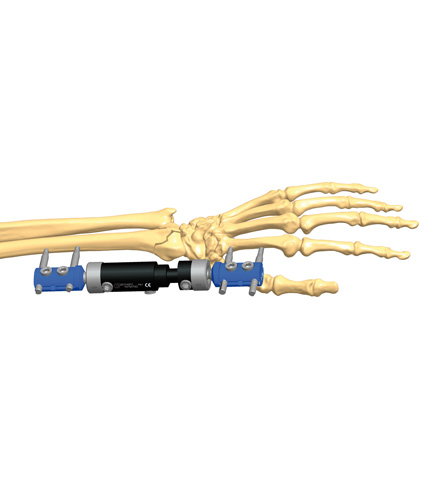
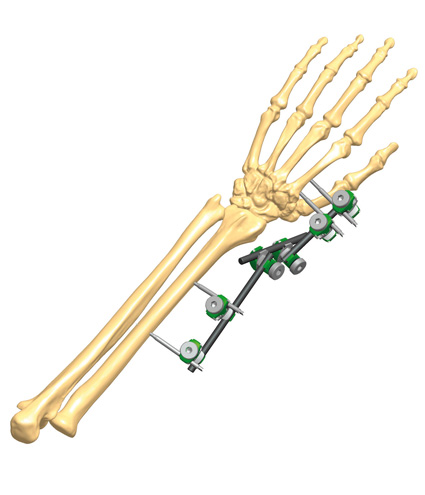
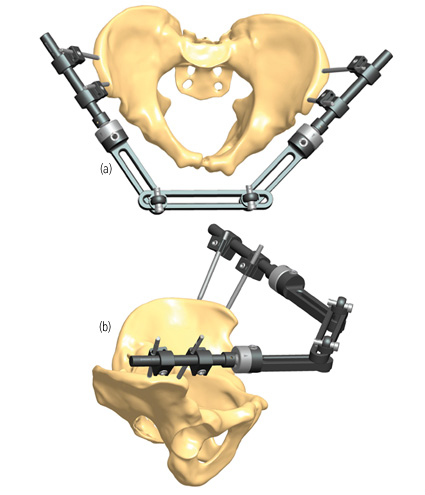
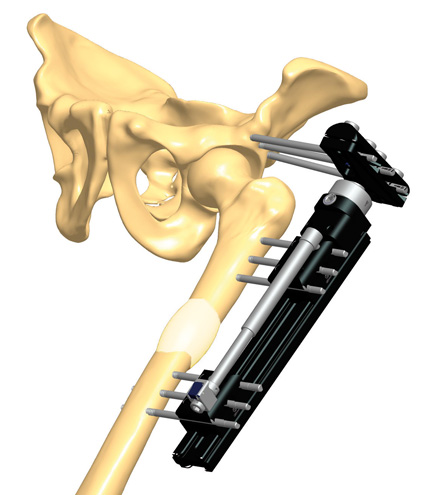
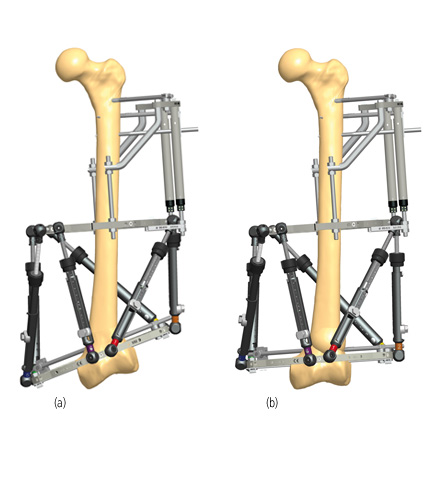
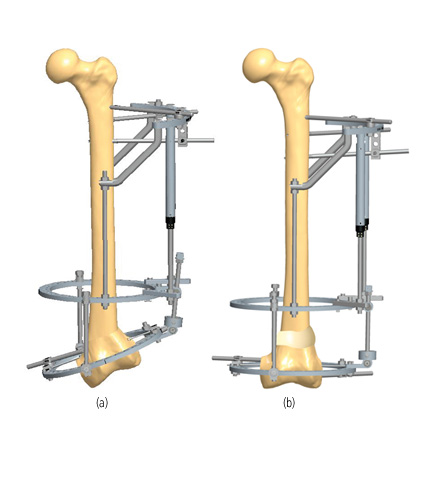
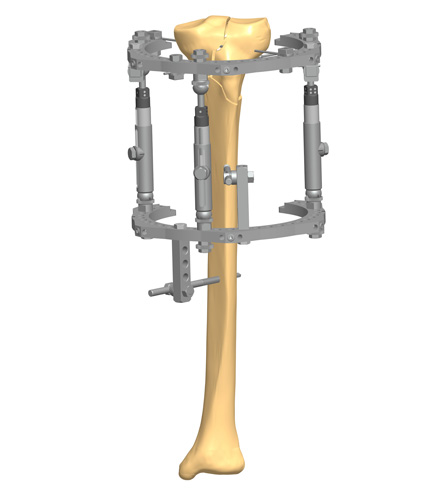
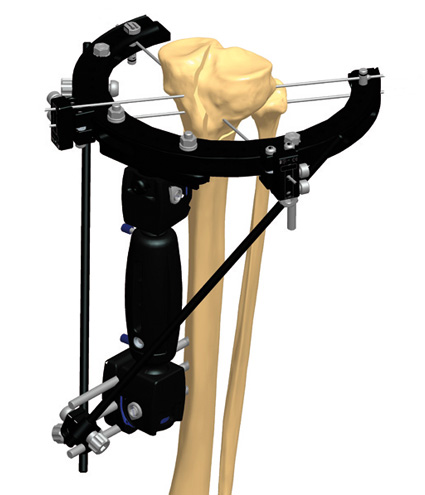
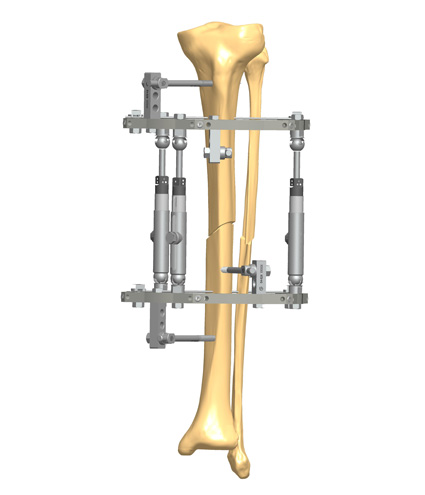
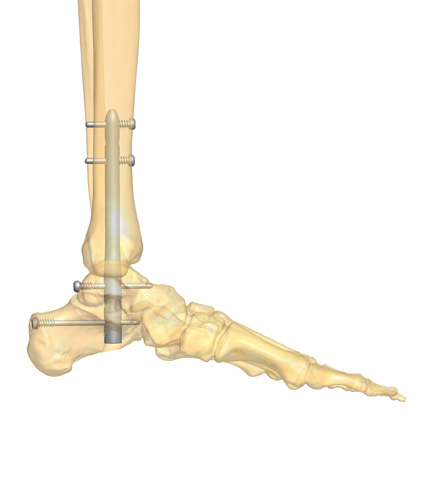
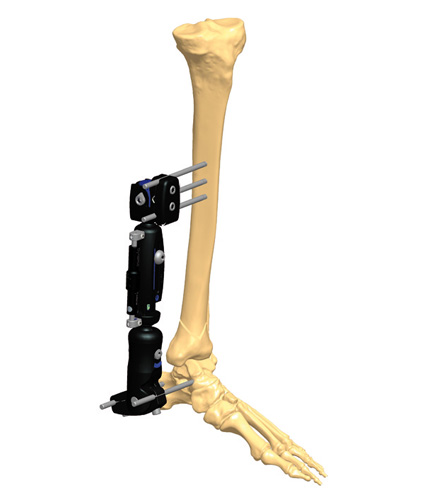
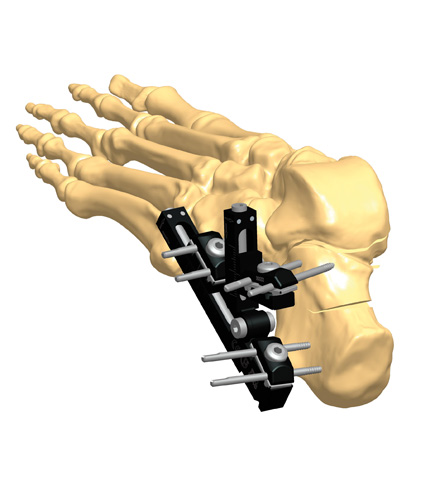
External fixation: in most trauma cases, it is a great way to treat fractures, but the surgeon has to respect some golden rules: know and follow the principles that are at the basis of the external fixation. Either it is temporary and will be removed in a few weeks, or it is going to be the definitive therapeutic option. External fixation must be applied in a correct and stable way, always controlling the anatomic alignment. External fixation is recommended in the presence of open fractures with contamination or impending compartment syndrome. It provides adequate stability, especially with comminution zones or oblique fractures.(3)
For some experts, external fixation is based on a minimally invasive concept, as it requires minimal excision and all the metal of the frame is removed at the treatment’s end. It is a simple and reliable method, with low complication rates as compared with other methods.
Four key points should be always considered by surgeons when treating a fracture: 1) soft tissue is a major priority, and vascular blood supply is critical to the subcutaneous tissues; 2) alignment is mandatory; 3) find a balance regarding joint reduction; and 4) early rehabilitation to recover patient’s limb functionality.
References
- Hohloch L, Konstantinidis L et al. 2015. Biomechanical evaluation of the new technique for external fixation of unstable sopracondylar humerus fractures in children. Technol Health Care; 23(4):453-61.
- Qingyu Z, Fanxiao L et al. 2016. Internal versus External Fixation for The Treatment of Distal Radial Fractures. Medicine (Baltimore); 95(9):e2945.
- Li WC, Meng QX et al. 2018. Biomechanical analysis between Orthofix external fixator and different K-wire configurations for pediatric supracondylar humerus fractures. J Orthop Surg Res; 13(1):188.