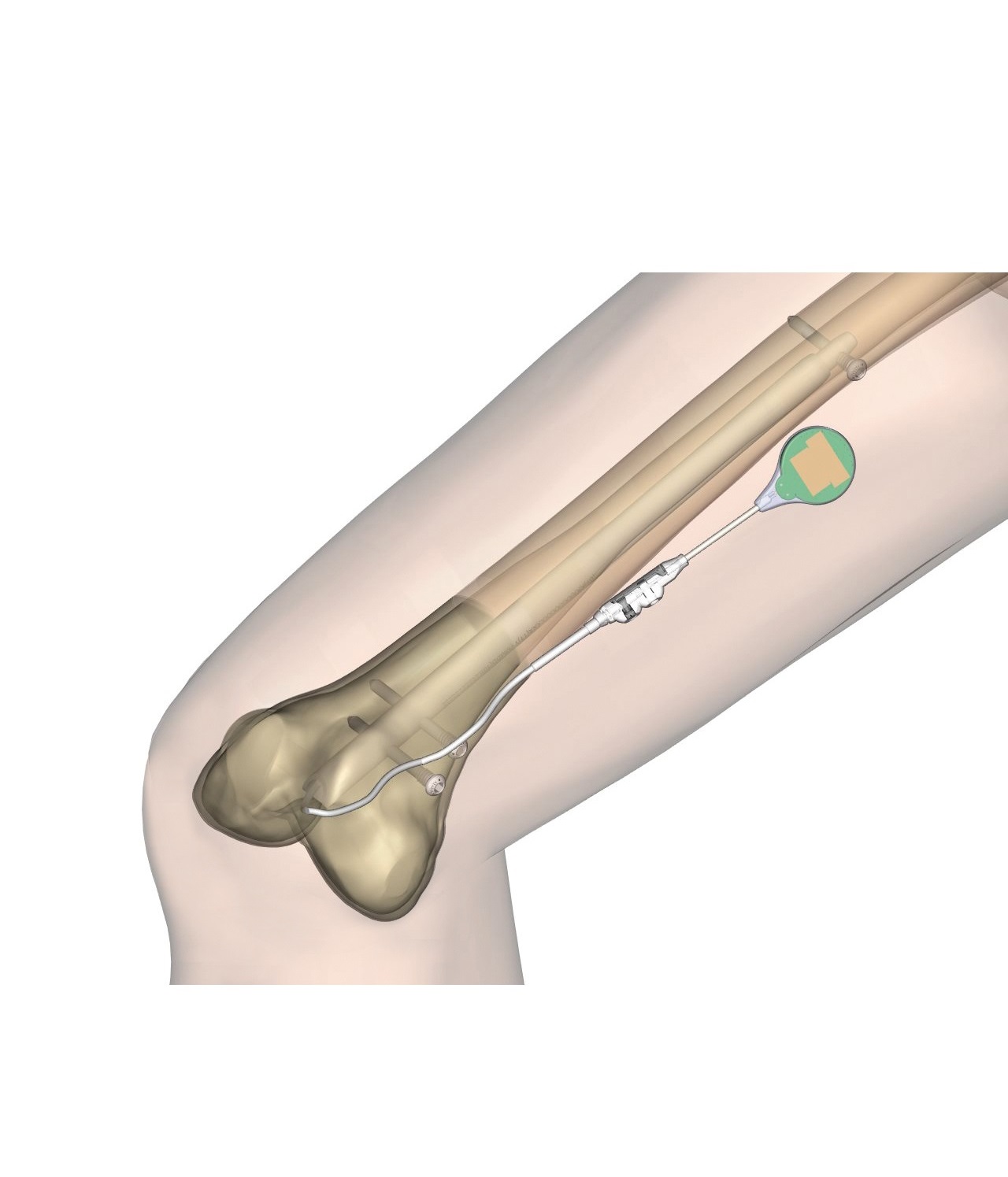
When an orthopedic surgeon has to perform a bone deformity correction, he or she may choose to apply an extrinsic method of correction such us an external fixator, or an intrinsic one, such us an intramedullary nail. In both cases, a surgeon will always have to consider the patient’s bone quality through three dimensional parameters: length, alignment and torsion, and accurately the entire 3D correction process. If using an intramedullary nail, an effective planning method is the Reverse Planning Method (RPM) developed by Prof. Rainer Baumgart in 2009.(1)
The RPM is a safe and successful intrinsic procedure for many bone correction situations – particularly when operating on the tibia and femur together at the same surgery. When planning in reverse, one starts with the end goal and works their way backwards to develop the operative plan. The RPM is a visual method that shows the surgeon exactly how to proceed to reach the final, optimal result. There is a fundamental difference between an extrinsic method of deformity correction and an intrinsic system: the first looks at the bone from outside – essentially, the bone’s layer – while the second one looks at the bone from inside.
In the case of a lower limb length discrepancy, the mechanical axis as well as the bone and joint orientation have to be geometrically measured. Some technical considerations like the entry point of the nail, the diameter of the diaphyseal canal, the curvature of the bone, the apex of deformity, the level of osteotomy, and the creation of an adequate bone segment size to allow for stable locking to the intramedullary nail, are accommodated. These well-defined measurements represent the situation as it is, and allow the surgeon to figure out how it will be at the end of surgery. A surgeon will know exactly where to ream and how to enter and place the nail in the bone canal safely.
Regarding the osteotomy point (where the bone has to be cut) when applying an intramedullary nail, this may not pass through the CORA (Center of Rotation of Angulation).(1)
Some orthopedic surgeons may use a software to pre-plan their surgery. Using a software is time-saving and allows the surgeon to compare the post-operative X-rays with the pre-operative ones. It is also useful for patient’s data record and further research.(2)
Some experts’ recommendations are the following:
- An accurate pre-operative planning is important to obtain a good result. Pre-planning is fundamental even if the correction to be obtained is moderate, and small measurements may seem clinically irrelevant. For instance, when doing lengthening, a surgeon should always consider the automatic valgisation that the nail causes, usually shifting the bone to valgus. This phenomenon may meet the patient’s needs in the case of a varus correction, but not in all cases. Pre-planning is always mandatory in order to prevent errors.
- An extra intra-operative alignment check (ref. the anatomical axis), using a grid, must always be performed.
- Compare post-operative results with pre-operative planning.
- If using intramedullary nailing, forget CORA!
- In the femur, a retrograde approach is technically less demanding, and it allows to correct wider deformities, 30° and more, compared to an antegrade approach.(3)
References
- Baumgart R 2009. The Reverse Planning Method for Lengthening of the Lower Limb Using a Straight Intramedullary Nail with or without Deformity Correction. A New Method. Operative Orthopädie und Traumatologie; 21(2):221-33.
- Atesok K, Galos D et al. 2015. Preoperative Planning in Orthopaedic Surgery. Current Practice and Evolving Applications. Bull Hosp Jt Dis; 73(4):257-68.
- Chan K Yu, Vivek A Singh et al. 2007. Antegrade Versus Retrograde Locked Intramedullary Nailing for Femoral Fractures: Which is Better?. Eur J Trauma Emerg Surg; 33:135-40.